Содержание
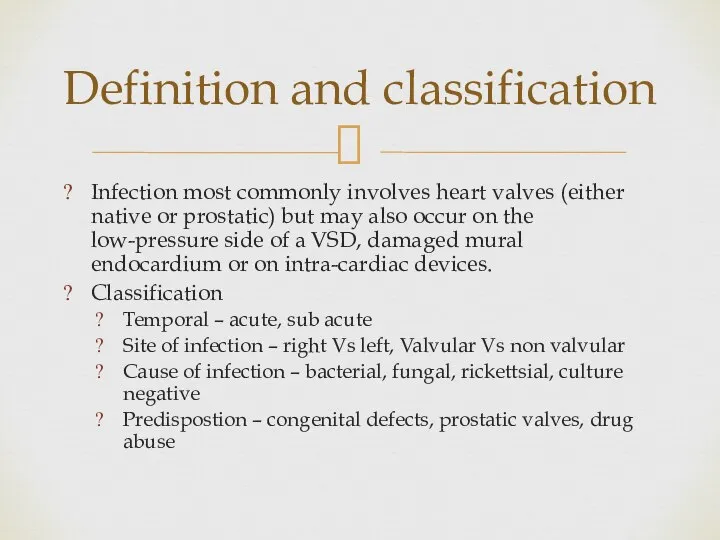
- 2. Infection most commonly involves heart valves (either native or prostatic) but may also occur on the
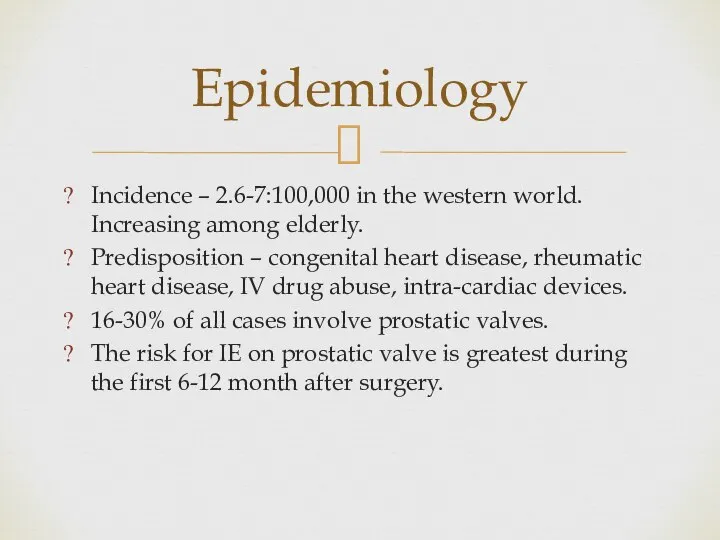
- 3. Incidence – 2.6-7:100,000 in the western world. Increasing among elderly. Predisposition – congenital heart disease, rheumatic
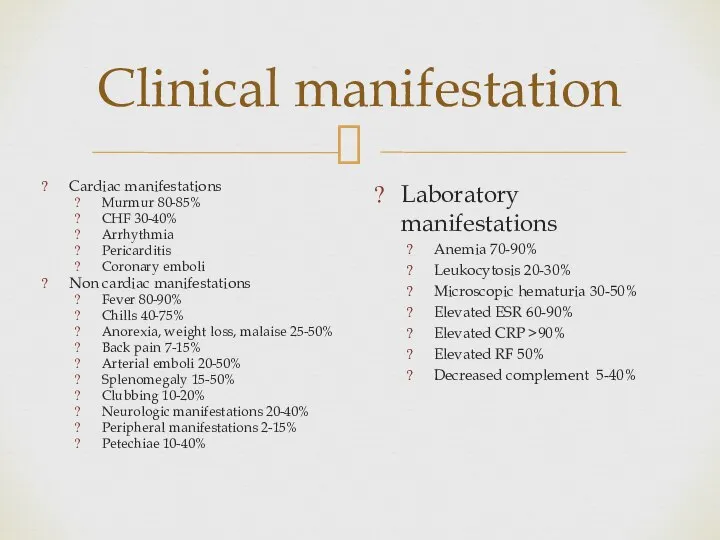
- 4. Clinical manifestation Cardiac manifestations Murmur 80-85% CHF 30-40% Arrhythmia Pericarditis Coronary emboli Non cardiac manifestations Fever
- 5. Clinical manifestations
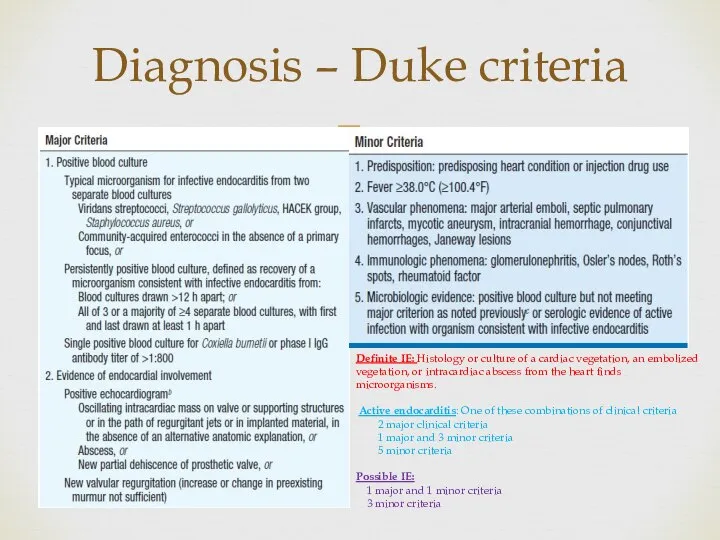
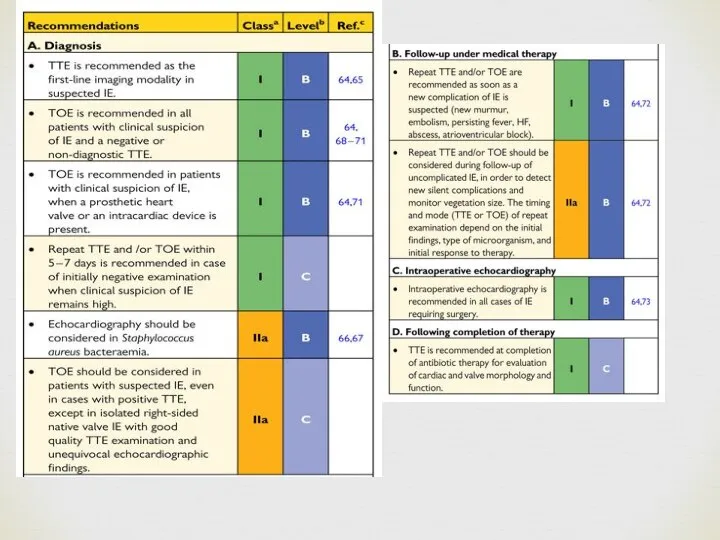
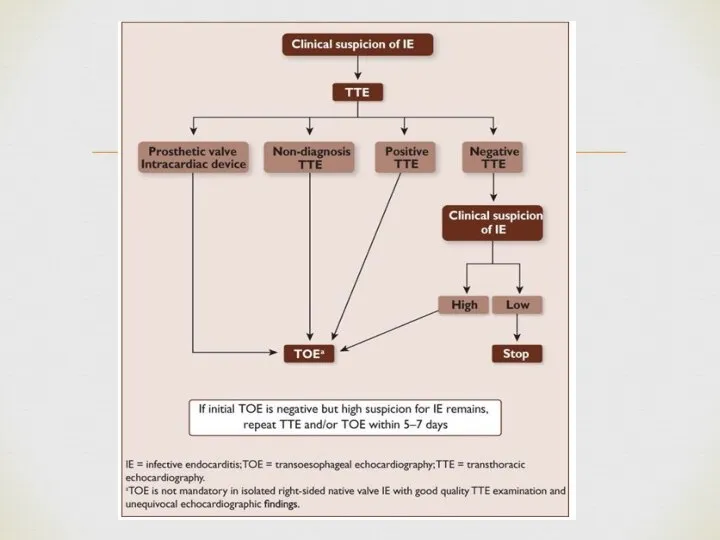
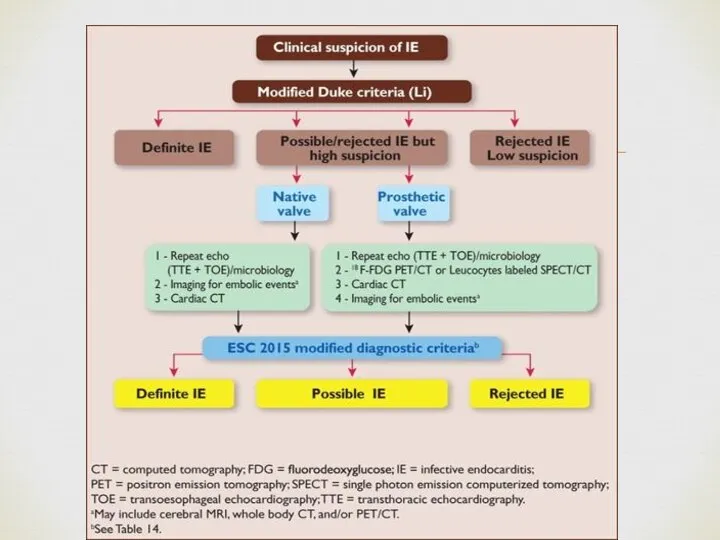
- 6. Diagnosis – Duke criteria Definite IE: Histology or culture of a cardiac vegetation, an embolized vegetation,
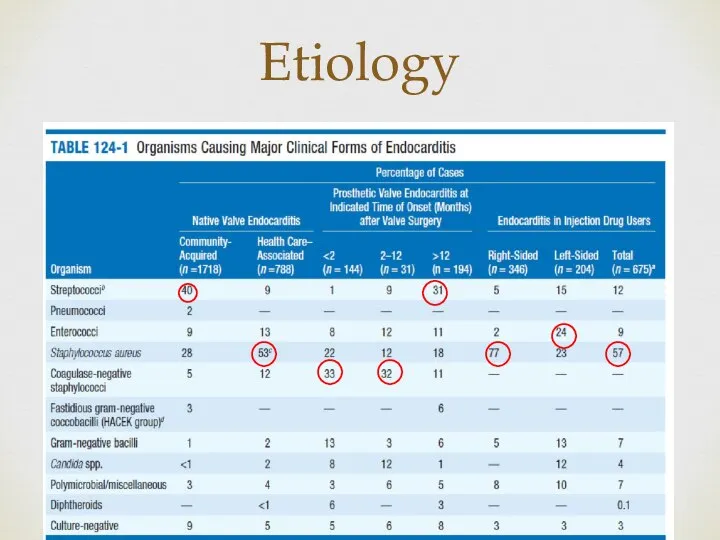
- 10. Etiology
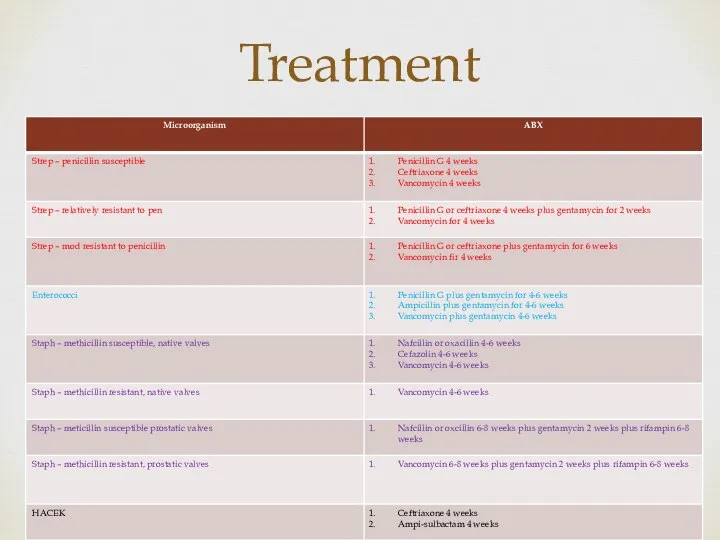
- 11. Treatment
- 12. B. quintana and B. henselae are the most common bartonella spp. implicated in endocarditis. Native valves
- 13. C. brunetti Gram neg cocco-bacillus Primary sources – cattle, sheep and goats Incidence – 24-54 cases
- 14. Main complications of left-sided valve infective endocarditis and their management HF is the most frequent and
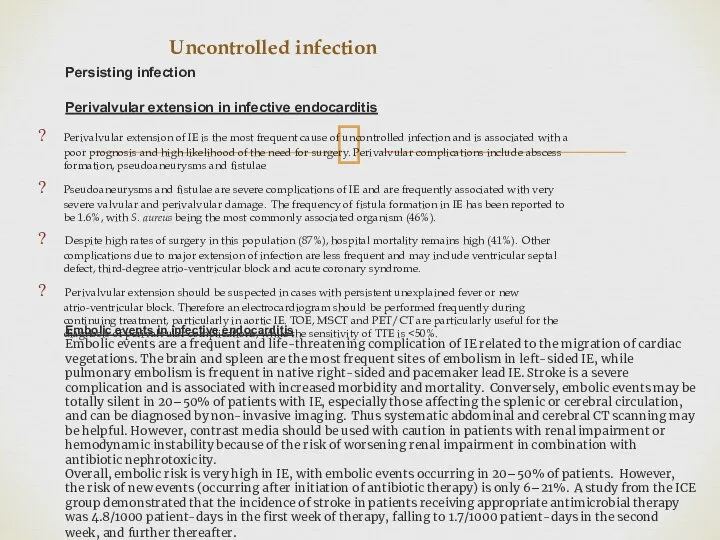
- 15. Uncontrolled infection Perivalvular extension of IE is the most frequent cause of uncontrolled infection and is
- 16. Neurological complications Symptomatic neurological events develop in 15–30% of all patients with IE and additional silent
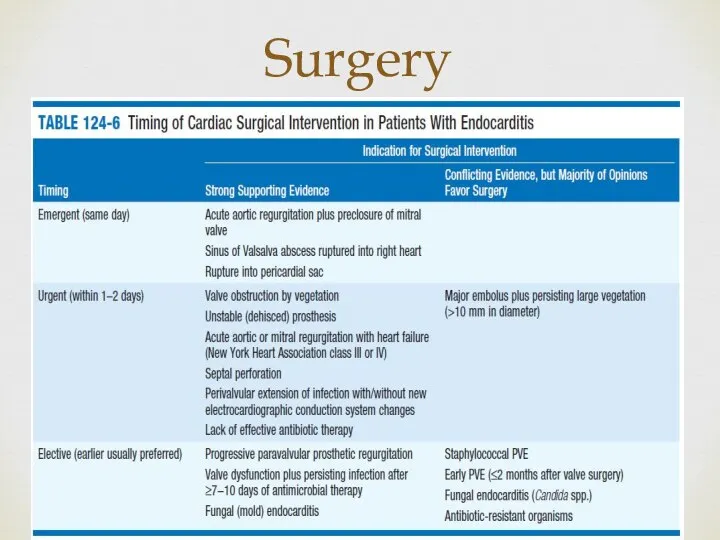
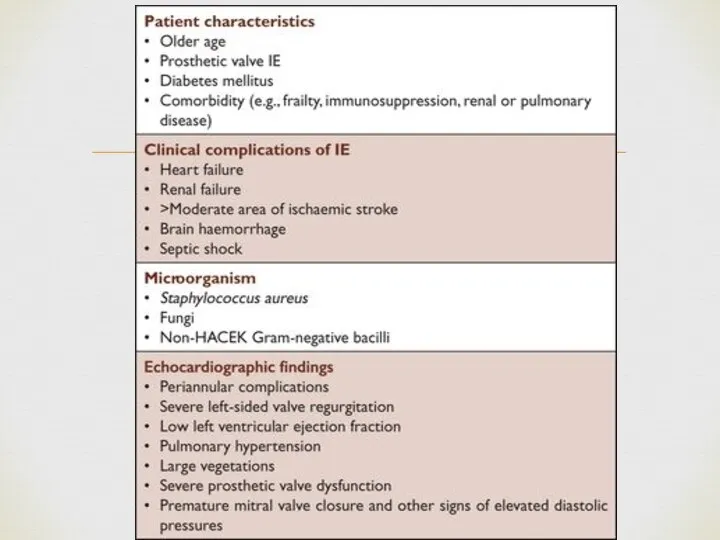
- 17. Surgery
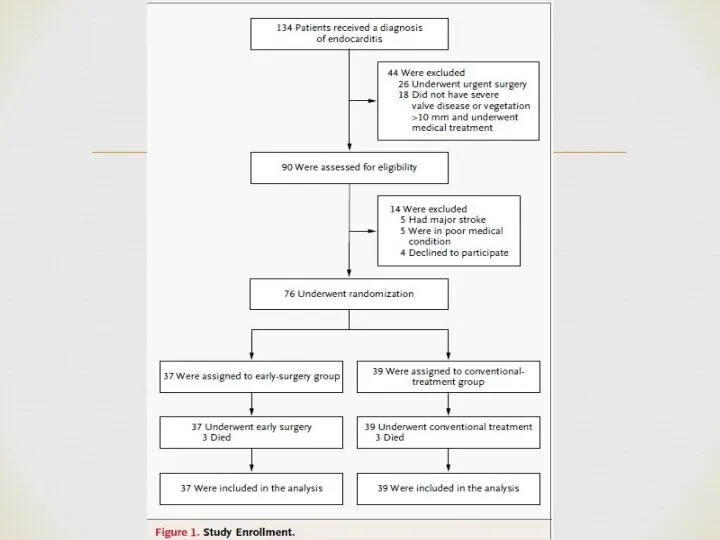
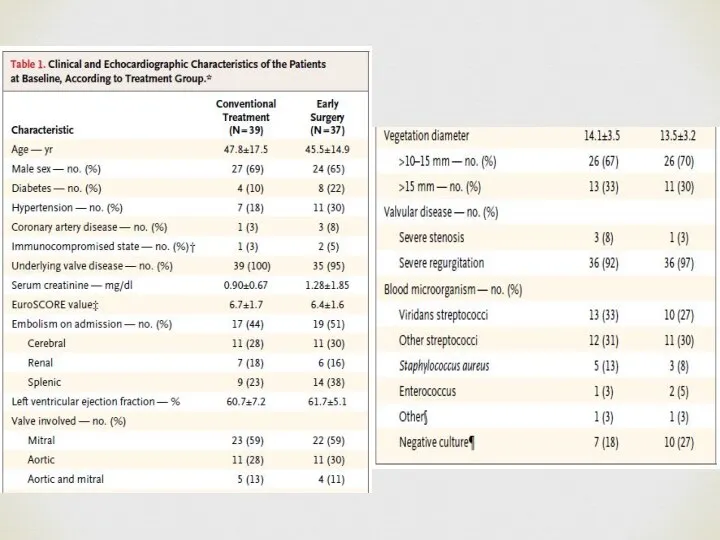
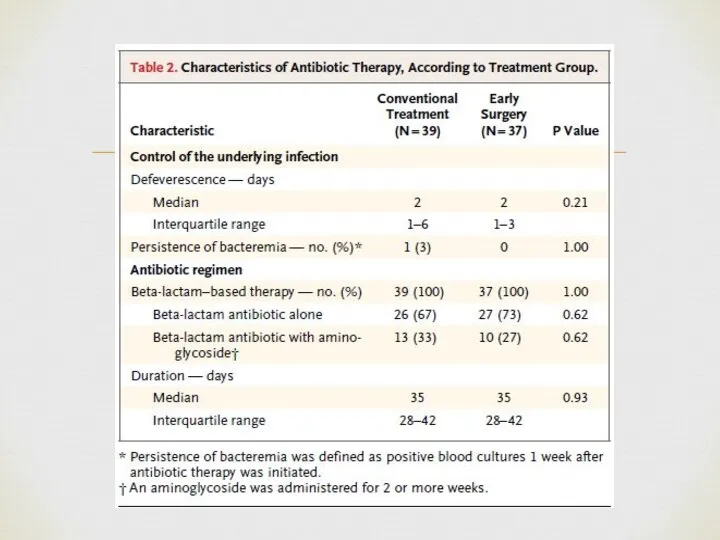
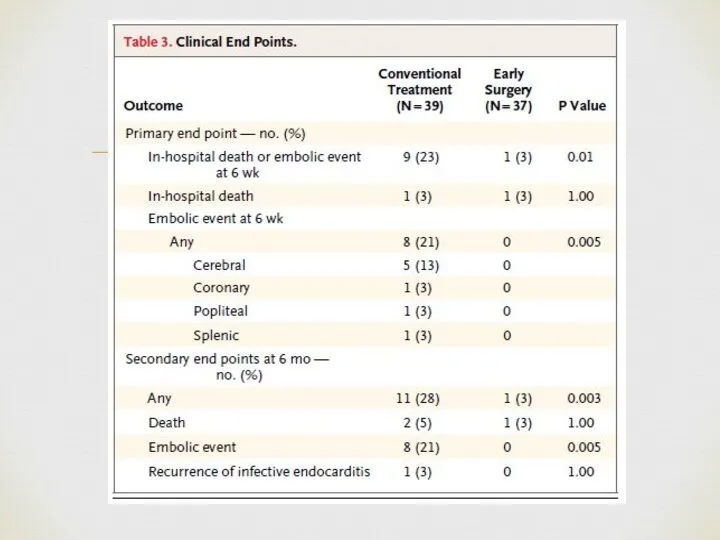
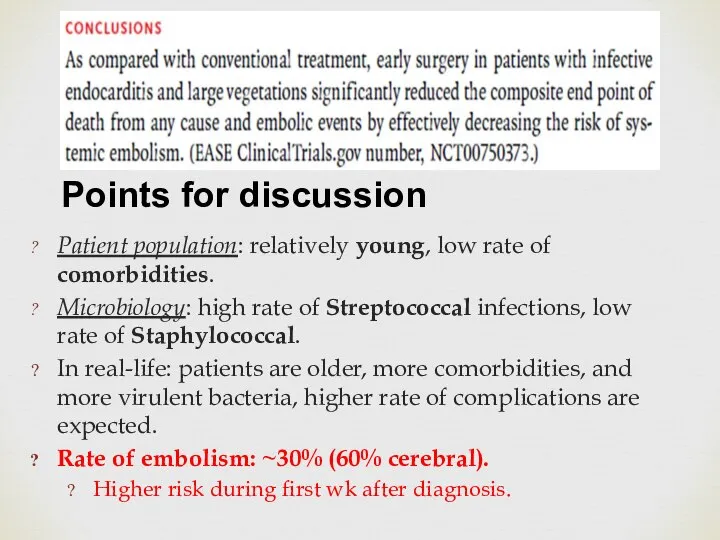
- 24. Patient population: relatively young, low rate of comorbidities. Microbiology: high rate of Streptococcal infections, low rate
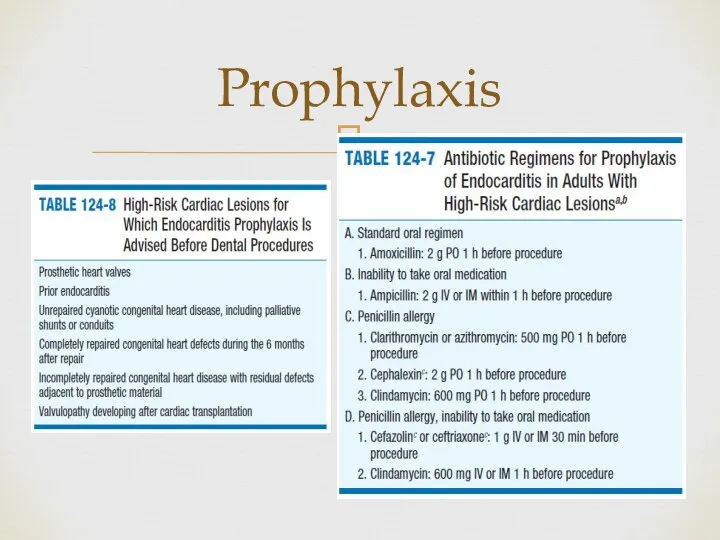
- 25. Prophylaxis
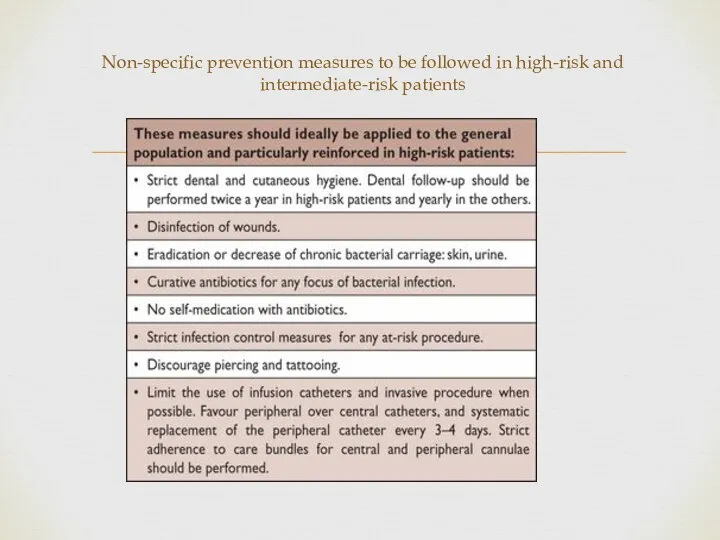
- 26. Non-specific prevention measures to be followed in high-risk and intermediate-risk patients
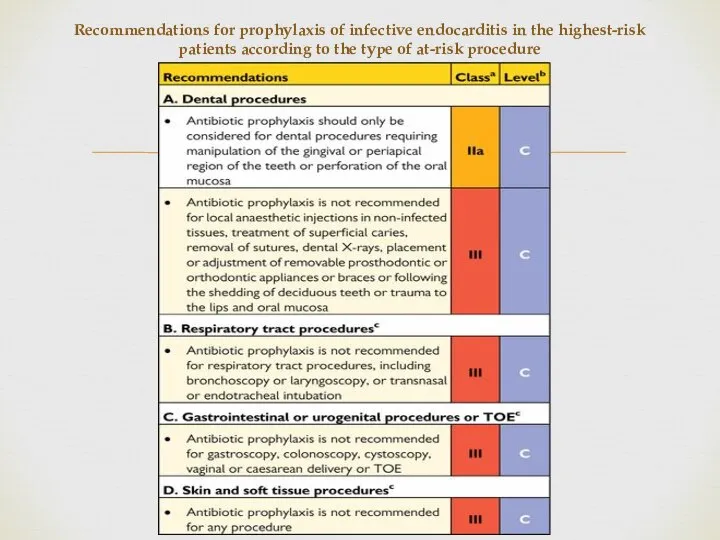
- 27. Recommendations for prophylaxis of infective endocarditis in the highest-risk patients according to the type of at-risk
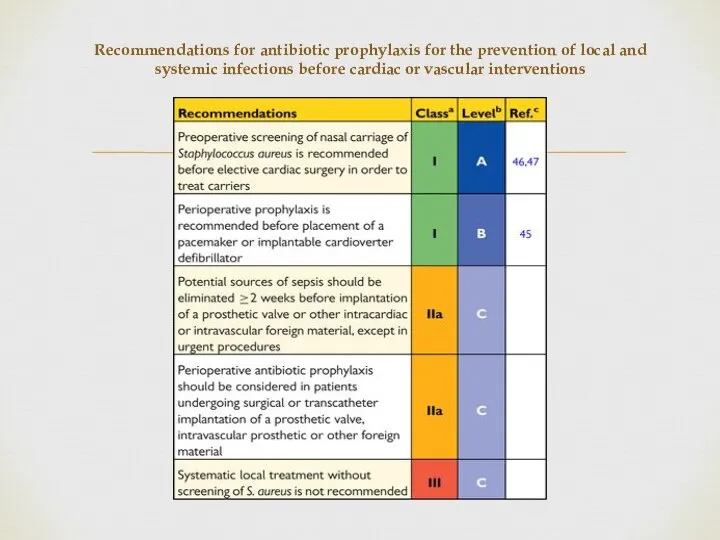
- 28. Recommendations for antibiotic prophylaxis for the prevention of local and systemic infections before cardiac or vascular
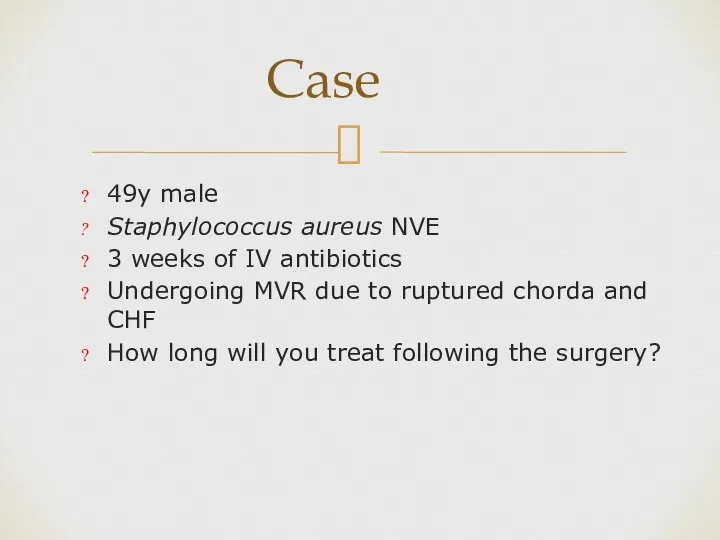
- 29. 49y male Staphylococcus aureus NVE 3 weeks of IV antibiotics Undergoing MVR due to ruptured chorda
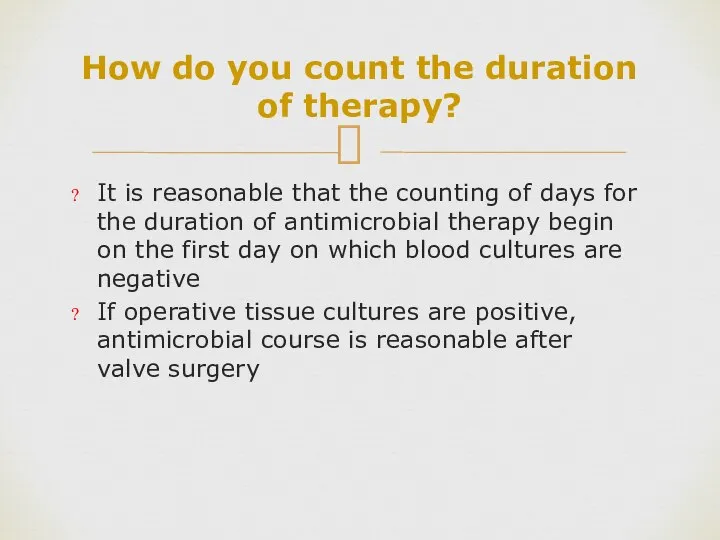
- 30. How do you count the duration of therapy? It is reasonable that the counting of days
- 32. Скачать презентацию


 Фармакогностический анализ плодов фенхеля
Фармакогностический анализ плодов фенхеля Резус-сенсибилизация. Гемолитическая болезнь плода
Резус-сенсибилизация. Гемолитическая болезнь плода Нарушение регуляции вегетативного тонуса при острой цереброваскулярной патологии
Нарушение регуляции вегетативного тонуса при острой цереброваскулярной патологии Болезни, передаваемые половым путем. Меры профилактики
Болезни, передаваемые половым путем. Меры профилактики Работа с людьми с последствиями детского церебрального паралича (ДЦП)
Работа с людьми с последствиями детского церебрального паралича (ДЦП) Аптечные организации, обслуживающие амбулаторных больных
Аптечные организации, обслуживающие амбулаторных больных Пищеварение и всасывание в кишечнике
Пищеварение и всасывание в кишечнике Системные васкулиты
Системные васкулиты Жобалық жабылымға байланысты өнімділікті (шикізат қорының тығыздығын) анықтау әдістемесі
Жобалық жабылымға байланысты өнімділікті (шикізат қорының тығыздығын) анықтау әдістемесі Временная остановка кровотечения наложением давящей повязки, жгута, закрутки
Временная остановка кровотечения наложением давящей повязки, жгута, закрутки Синдром Острого живота
Синдром Острого живота Патология мочевыделительной системы
Патология мочевыделительной системы Стенокардия. Заболевания сердечно-сосудистой системы
Стенокардия. Заболевания сердечно-сосудистой системы Фармацевтическая экспертиза рецептов на лекарственные средства
Фармацевтическая экспертиза рецептов на лекарственные средства Цитостати́ческие препара́ты (цитоста́тики)
Цитостати́ческие препара́ты (цитоста́тики) Черепно-мозговые травмы. Переломы свода черепа. Переломы верхней и нижней челюсти. Переломы носа
Черепно-мозговые травмы. Переломы свода черепа. Переломы верхней и нижней челюсти. Переломы носа Сестринская помощь при бешенстве и столбняке
Сестринская помощь при бешенстве и столбняке Клиническое применение роллов в контексте метода Фельденкрайз
Клиническое применение роллов в контексте метода Фельденкрайз Питание здорового ребёнка
Питание здорового ребёнка Хитозан и здоровье человека
Хитозан и здоровье человека Оказание качественной эффективной медицинской помощи путем достижения медицинской работниками доверия пациента
Оказание качественной эффективной медицинской помощи путем достижения медицинской работниками доверия пациента Астмалық статус
Астмалық статус (1)
(1) О вреде избыточного потребления сахара
О вреде избыточного потребления сахара Этиология и классификация аритмий. Основные группы антиаритмических препаратов. Принципы терапии экстрасистолии
Этиология и классификация аритмий. Основные группы антиаритмических препаратов. Принципы терапии экстрасистолии Hospitalization. Госпитализация
Hospitalization. Госпитализация Факторы препятствующие к проникновению и распространению инфекции. Сомкнутое состояние половой щели. Кислая среда влагалища
Факторы препятствующие к проникновению и распространению инфекции. Сомкнутое состояние половой щели. Кислая среда влагалища Злокачественные новообразования женских половых органов
Злокачественные новообразования женских половых органов