Содержание
- 2. 10% of patients presenting with VT have no apparent structural heart disease VT in structurally normal
- 3. NON–LIFE-THREATENING (TYPICALLY MONOMORPHIC) Classified on basis of site of origin Most common sites are ventricular outflow
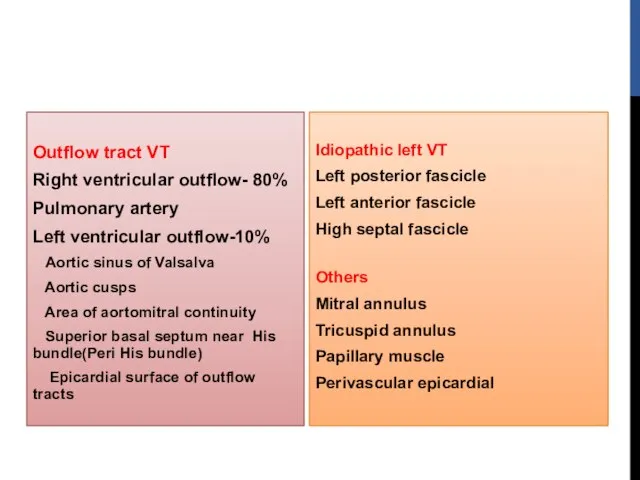
- 4. Idiopathic left VT Left posterior fascicle Left anterior fascicle High septal fascicle Others Mitral annulus Tricuspid
- 5. OUTFLOW TRACT VT Idiopathic VT originate most commonly in outflow tract area Nearly 80% of which
- 6. Phenotypes are a continuum of the same focal cellular process Premature ventricular complexes (PVCs) Nonsustained,repetitive monomorphic
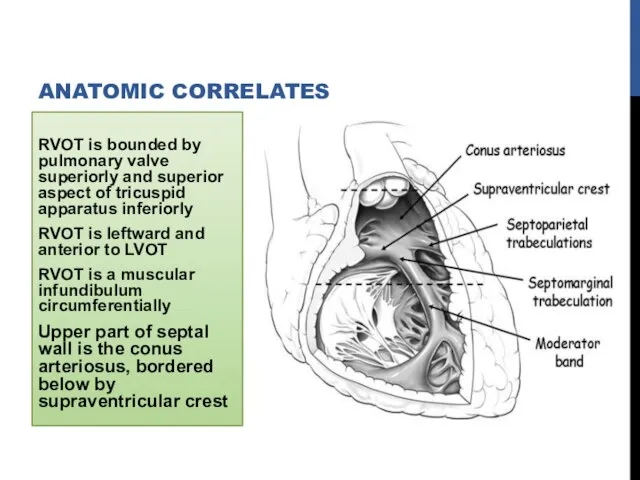
- 7. RVOT is bounded by pulmonary valve superiorly and superior aspect of tricuspid apparatus inferiorly RVOT is
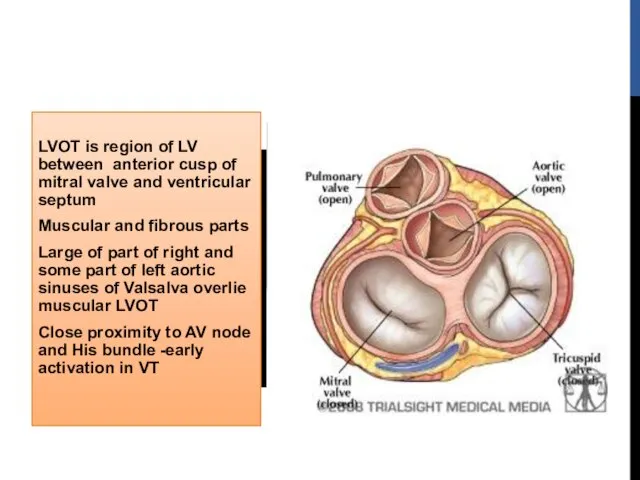
- 8. LVOT is region of LV between anterior cusp of mitral valve and ventricular septum Muscular and
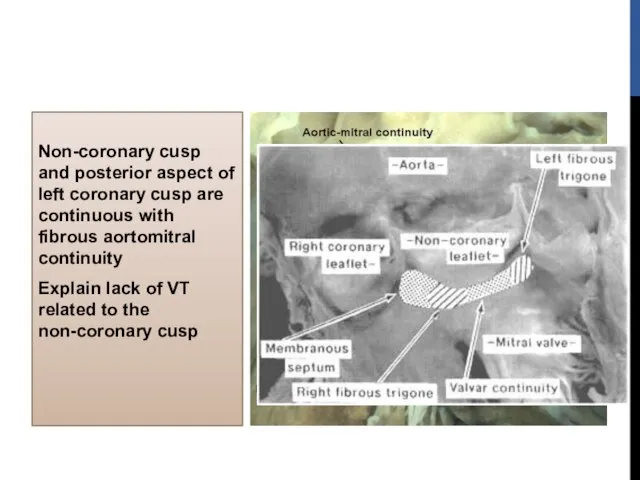
- 9. Non-coronary cusp and posterior aspect of left coronary cusp are continuous with fibrous aortomitral continuity Explain
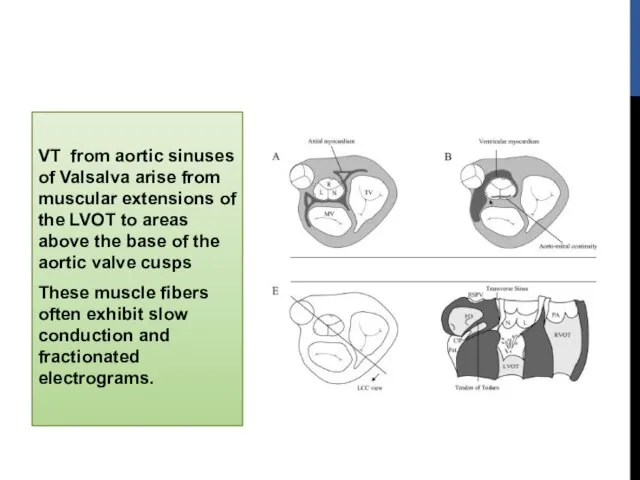
- 10. VT from aortic sinuses of Valsalva arise from muscular extensions of the LVOT to areas above
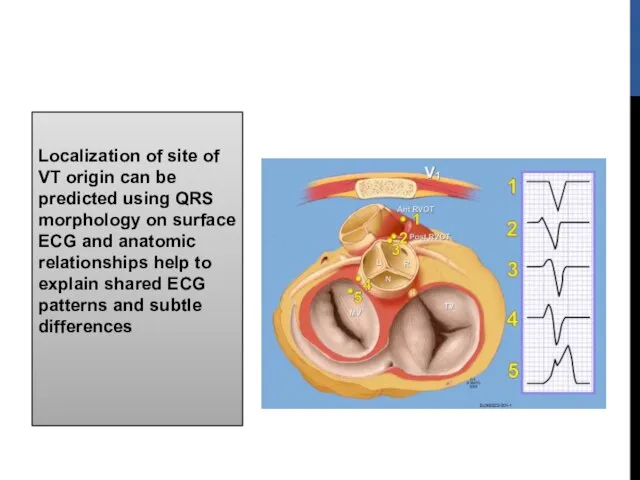
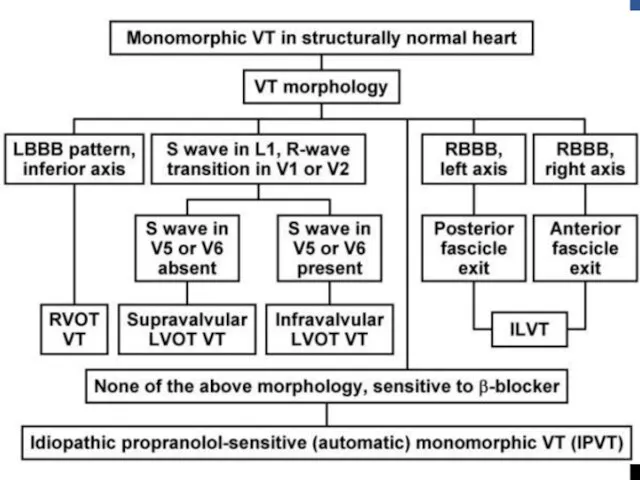
- 11. Localization of site of VT origin can be predicted using QRS morphology on surface ECG and
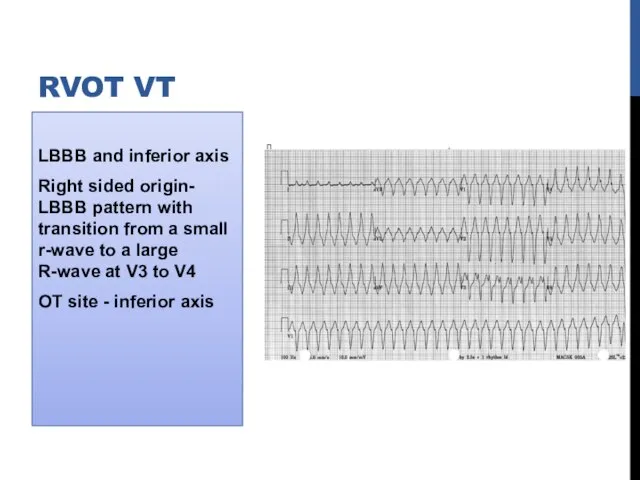
- 12. LBBB and inferior axis Right sided origin- LBBB pattern with transition from a small r-wave to
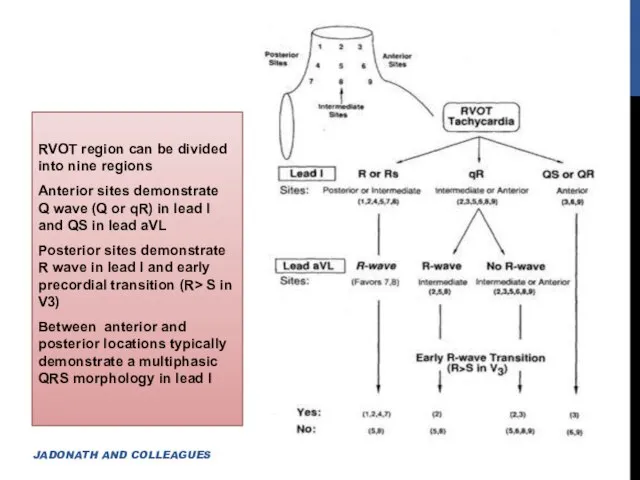
- 13. RVOT region can be divided into nine regions Anterior sites demonstrate Q wave (Q or qR)
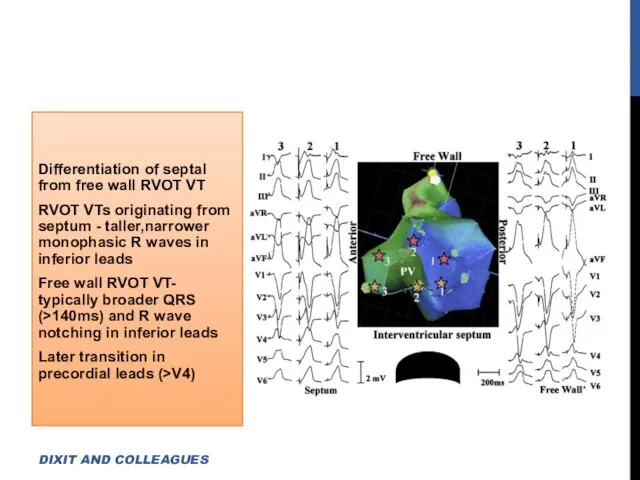
- 14. Differentiation of septal from free wall RVOT VT RVOT VTs originating from septum - taller,narrower monophasic
- 15. Anterior position of free wall relative to septum -Accounts for deeper S wave in lead V2
- 16. Approximately 1 cm above pulmonic valve Associated with a precordial transition in leads V3 or V4(PA
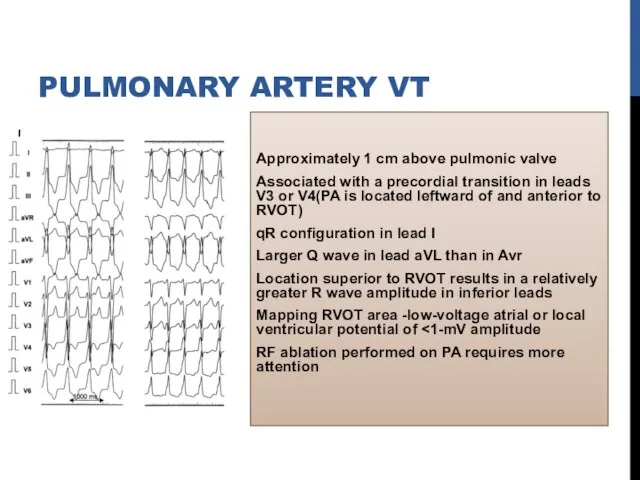
- 17. Atriofascicular fibers (Mahaim fibers) AVRT using Rt-sided accessory pathway VT after repair of TOF ARVD DIFFERENTIAL
- 18. ECG during VT shows S wave in lead I R-wave transition in lead V1or V2(Earlier precordial
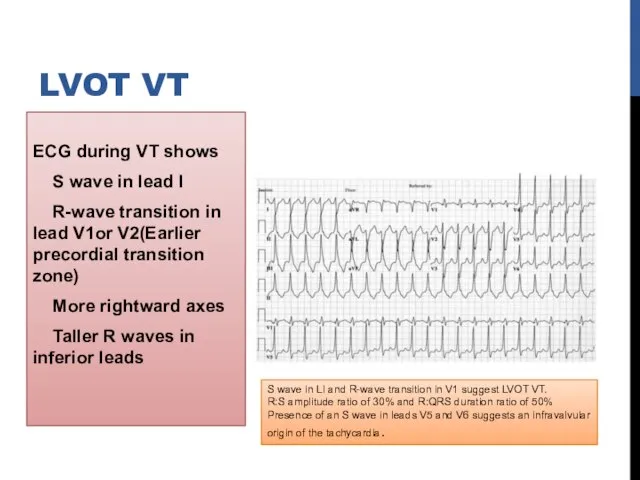
- 19. Shows one of the following depending on site of origin a)Basal left interventricular or septal origin
- 20. May originate from supravalvular or infravalvular endocardial region of coronary cusp of aortic valve Distinction is
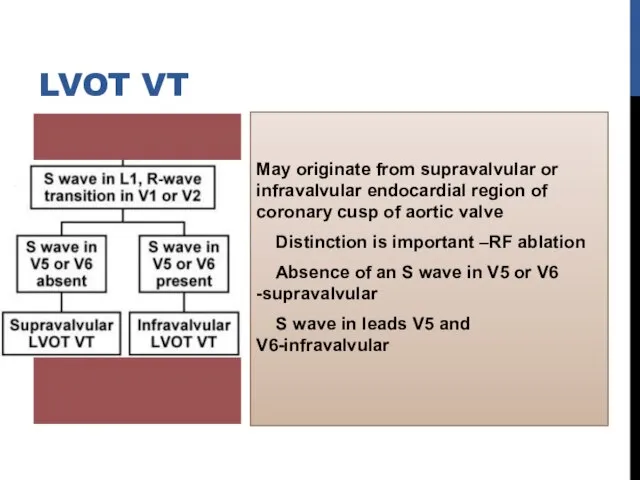
- 21. Depending on site of origin from right or left coronary cusp-LBBB or RBBB morphology AORTIC CUSP
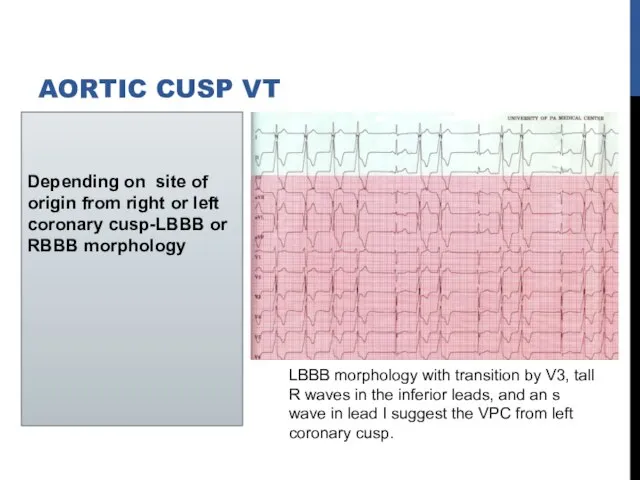
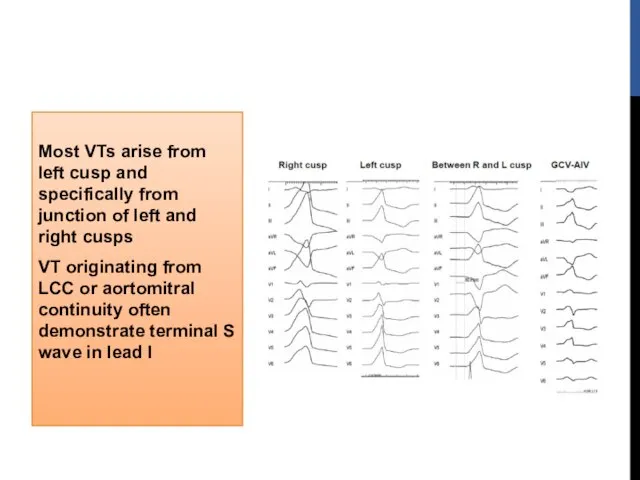
- 22. Most VTs arise from left cusp and specifically from junction of left and right cusps VT
- 23. RVOT VT Vs aortic cusp VT R wave duration and R/S wave amplitude ratio in leads
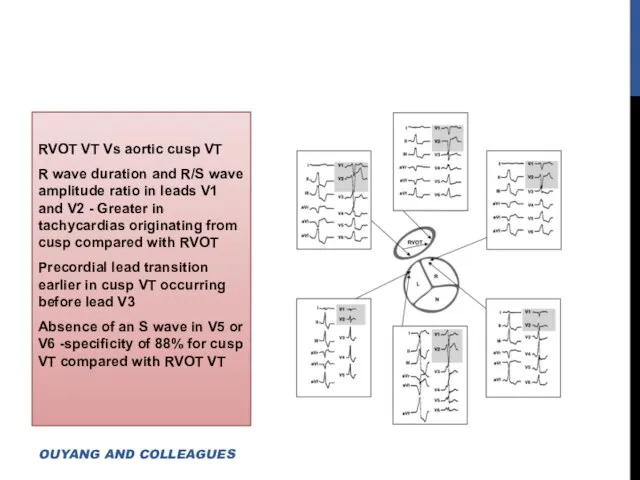
- 24. OTVT originate from epicardial locations 9%–13% of idiopathic VT Cluster along the course of the anterior
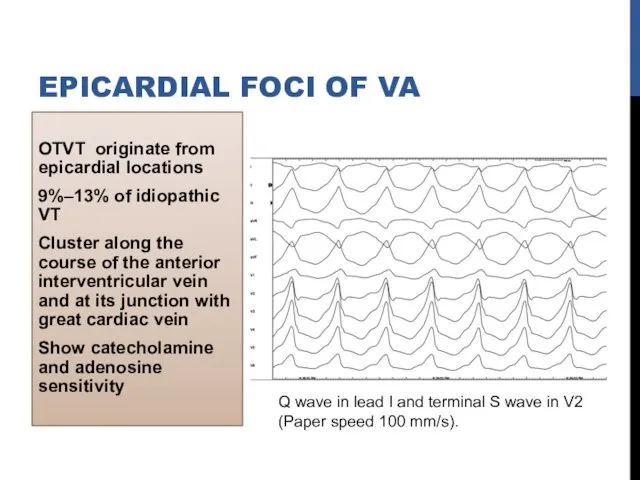
- 25. Psuedodelta wave Interval from earliest QRS activation to earliest fast deflection in precordial leads ( >
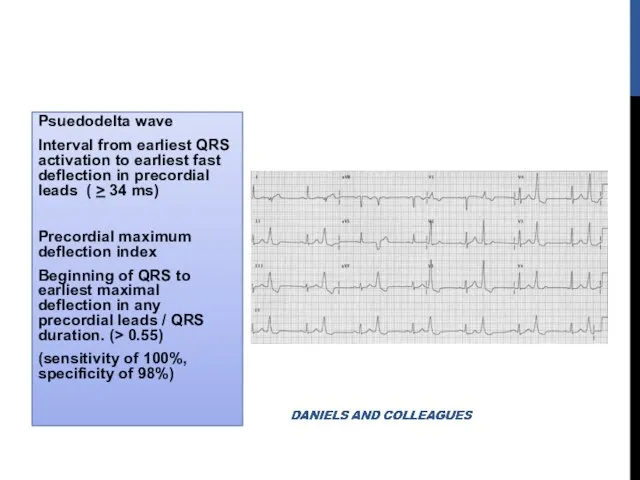
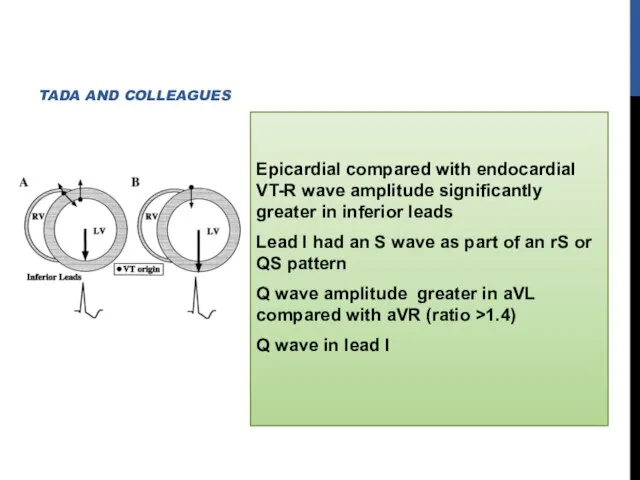
- 26. Epicardial compared with endocardial VT-R wave amplitude significantly greater in inferior leads Lead I had an
- 27. MITRAL ANNULUS, TRICUSPID ANNULUS PAPILLARY MUSCLE PERIVASCULAR EPICARDIAL ECTOPY
- 28. MITRAL ANNULAR VT Significant slurring of QRS complex onset resembling delta-wave Regardless of where along circumference
- 29. PVCs or VT also originate from RVOT along region of tricuspid annulus Most common site is
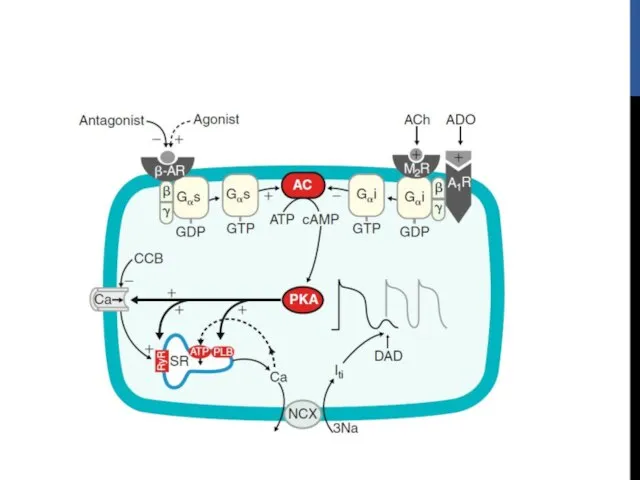
- 30. ELECTROPHYSIOLOGIC MECHANISM Outflow tract VT is due to triggered activity Secondary to cyclic AMP mediated DAD
- 32. CLINICAL FEATURES 20 and 40 years,Slight female preponderance May be asymptomatic but often present with palpitations,
- 33. TREATMENT May respond acutely to carotid sinus massage, Valsalva maneuvers or intravenous adenosine or verapamil Long-term
- 34. RFA When medical therapy is ineffective or not tolerated High success rate (>80%) Ablation of epicardial
- 35. Tachycardia localization 12-lead ECG Intracardiac activation Pace mapping
- 36. BIPOLAR ACTIVATION MAPPING
- 37. PACE MAPPING Useful because typically site of origin is focal and because underlying tissue is normal
- 38. ELECTROANATOMIC RE-CREATION OF 3D ANATOMY Helpful for catheter mapping and localization of site of origin Incessant
- 39. Predictors for successful ablation Single VT morphology Accurate pace maps Absence of a deltalike wave at
- 40. Some tachycardias arise from epicardium, necessitate ablation from great cardiac vein or epicardium itself using pericardial
- 41. Complications during outflow tract VT ablation are rare RBBB (1%) Cardiac perforation Damage to the coronary
- 42. IDIOPATHIC LEFT VT Three varieties left posterior fascicular VT -RBBB and LAD (90%) left anterior fascicular
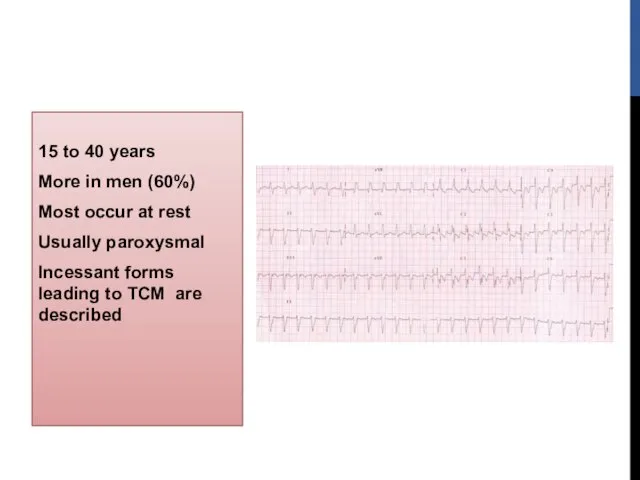
- 43. 15 to 40 years More in men (60%) Most occur at rest Usually paroxysmal Incessant forms
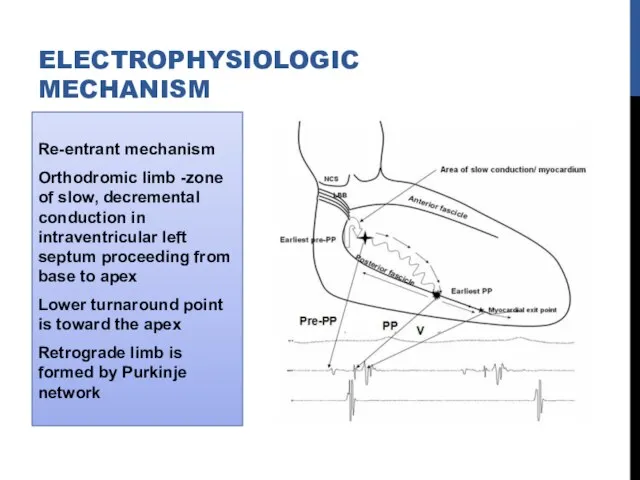
- 44. Re-entrant mechanism Orthodromic limb -zone of slow, decremental conduction in intraventricular left septum proceeding from base
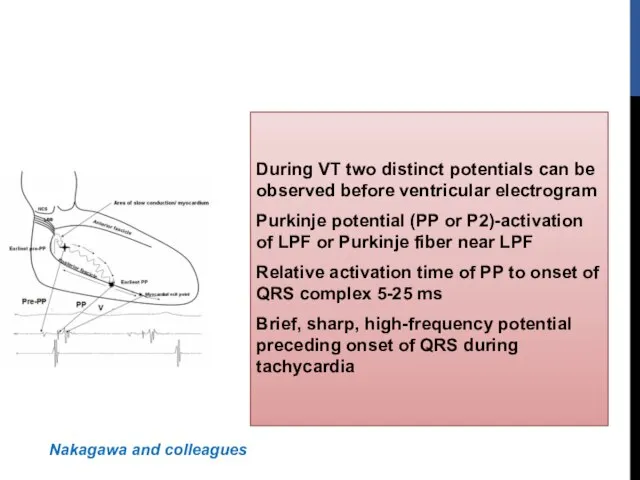
- 45. During VT two distinct potentials can be observed before ventricular electrogram Purkinje potential (PP or P2)-activation
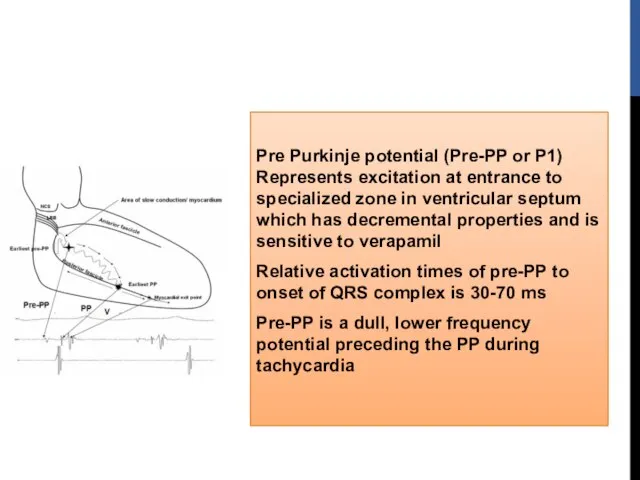
- 46. Pre Purkinje potential (Pre-PP or P1) Represents excitation at entrance to specialized zone in ventricular septum
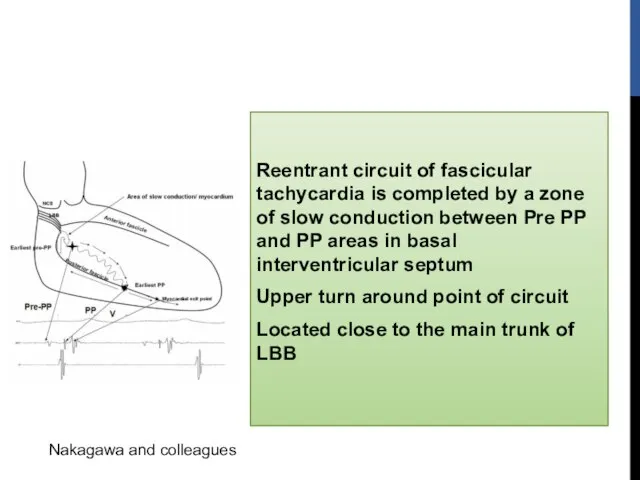
- 47. Reentrant circuit of fascicular tachycardia is completed by a zone of slow conduction between Pre PP
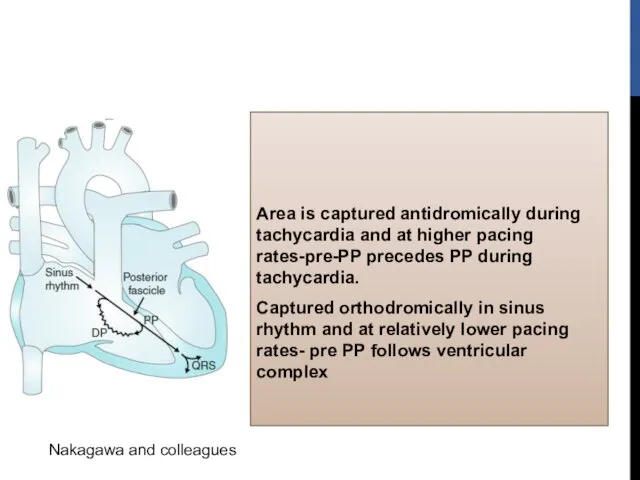
- 48. Area is captured antidromically during tachycardia and at higher pacing rates-pre-PP precedes PP during tachycardia. Captured
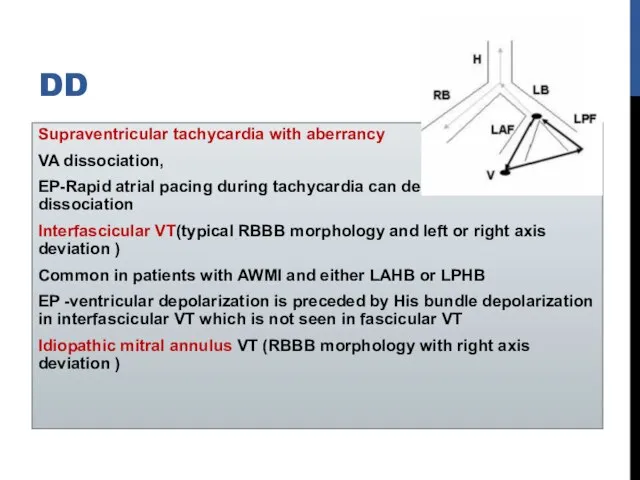
- 49. DD Supraventricular tachycardia with aberrancy VA dissociation, EP-Rapid atrial pacing during tachycardia can demonstrate AV dissociation
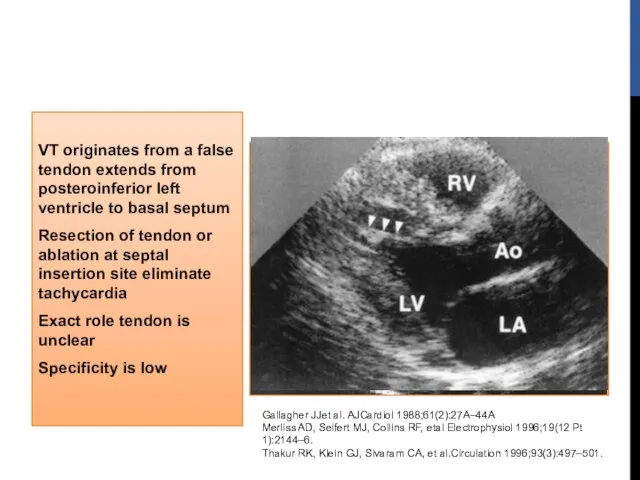
- 50. VT originates from a false tendon extends from posteroinferior left ventricle to basal septum Resection of
- 51. ECG Baseline 12-lead ECG is normal in most patients Exit near the area of the left
- 52. Long-term prognosis is very good Patients who have incessant tachycardia may develop tachycardia related cardiomyopathy Intravenous
- 53. RADIOFREQUENCY ABLATION Associated with significant symptoms or who are intolerant or resistant to medical therapy Strategies
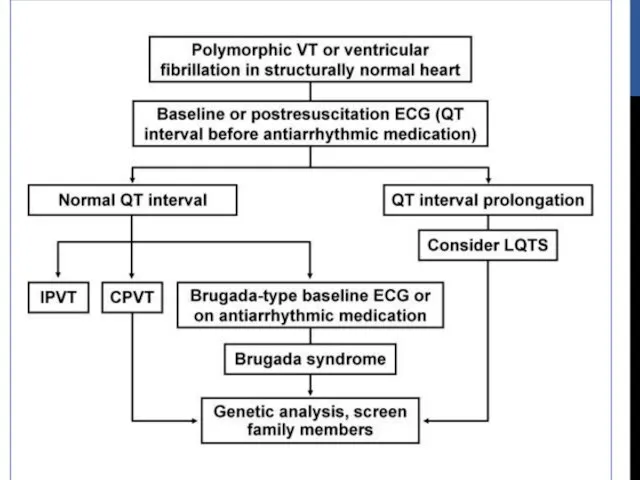
- 54. LIFE-THREATENING (TYPICALLY POLYMORPHIC VT) Rare Generally occurs with genetic ion channel disorders Associated with SCD Abnormalities
- 55. Long QT Syndrome Brugada Syndrome CPVT Short QT Syndrome LIFE-THREATENING (TYPICALLY POLYMORPHIC VT)
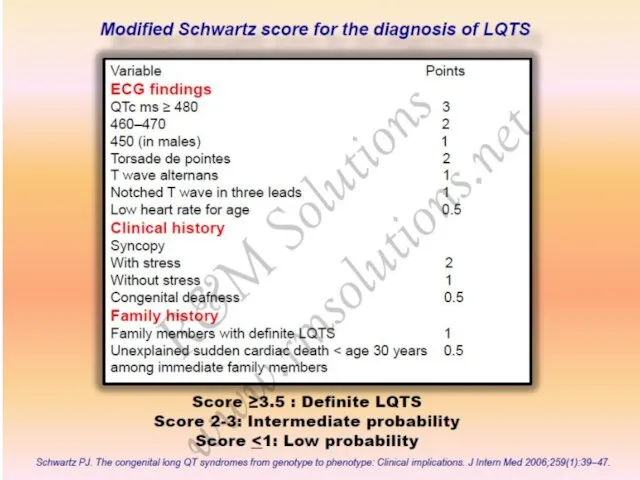
- 56. LONG QT SYNDROME Corrected QT interval 440 ms in men and 460 ms in women with
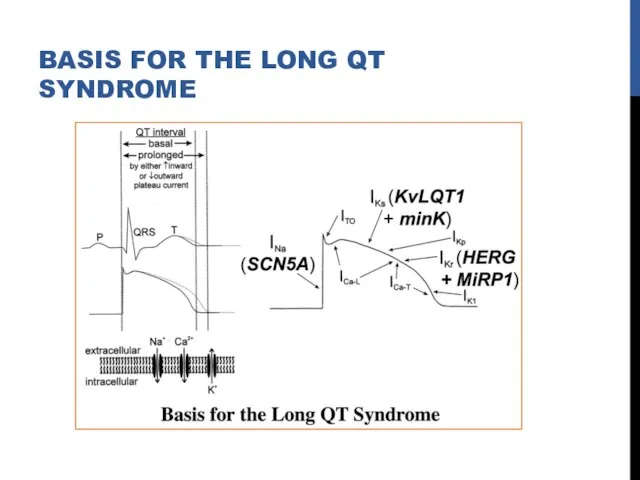
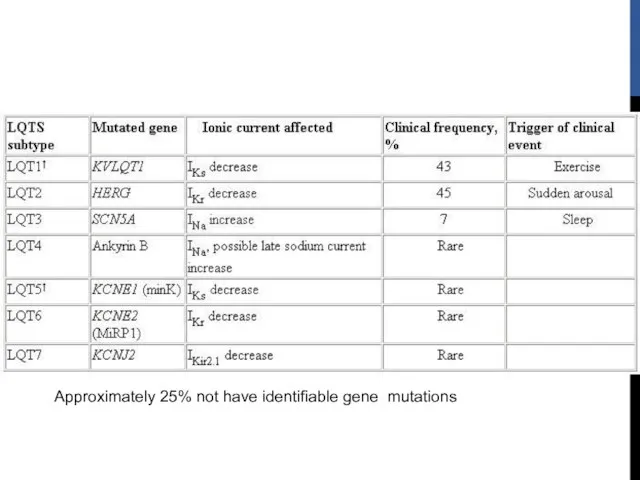
- 57. BASIS FOR THE LONG QT SYNDROME
- 58. Approximately 25% not have identifiable gene mutations
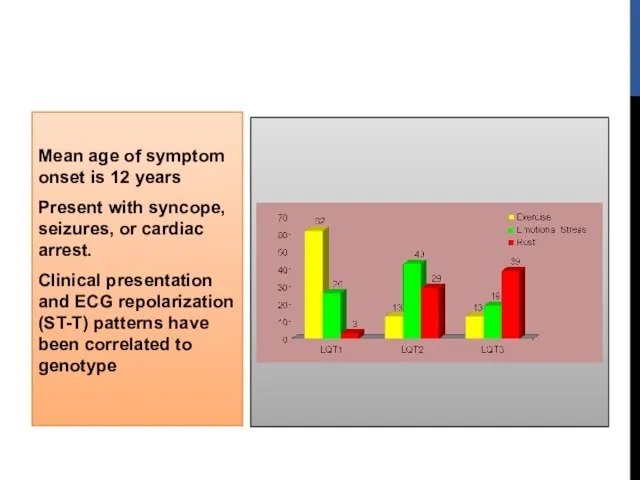
- 59. Mean age of symptom onset is 12 years Present with syncope, seizures, or cardiac arrest. Clinical
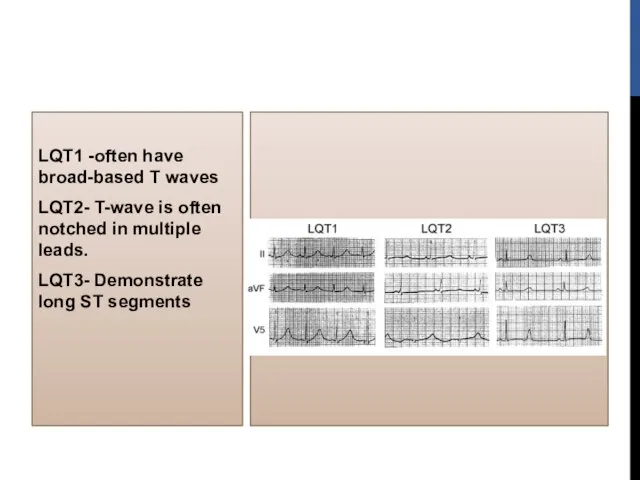
- 60. LQT1 -often have broad-based T waves LQT2- T-wave is often notched in multiple leads. LQT3- Demonstrate
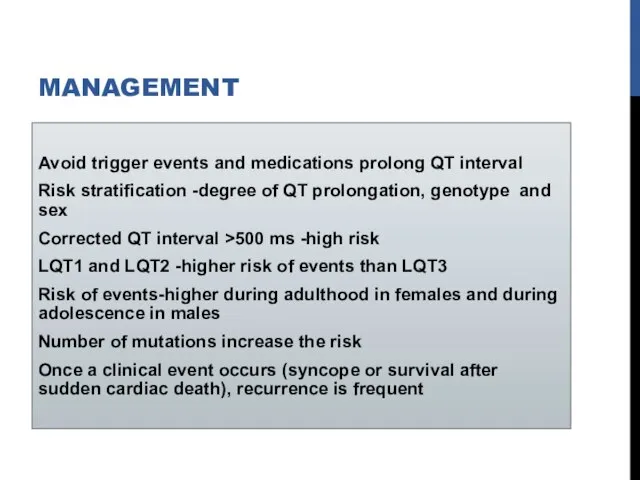
- 62. MANAGEMENT Avoid trigger events and medications prolong QT interval Risk stratification -degree of QT prolongation, genotype
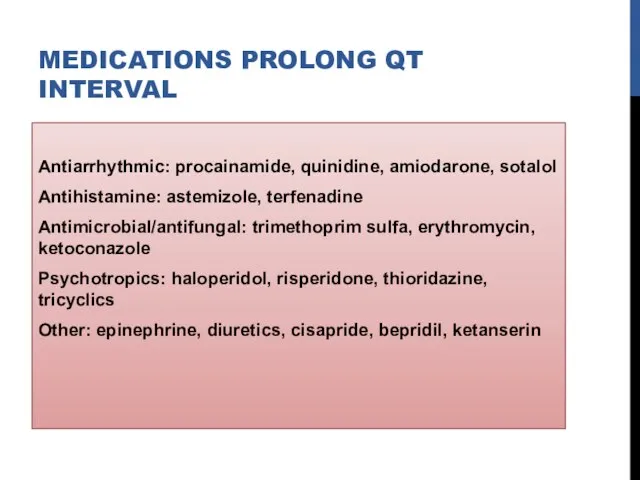
- 63. MEDICATIONS PROLONG QT INTERVAL Antiarrhythmic: procainamide, quinidine, amiodarone, sotalol Antihistamine: astemizole, terfenadine Antimicrobial/antifungal: trimethoprim sulfa, erythromycin,
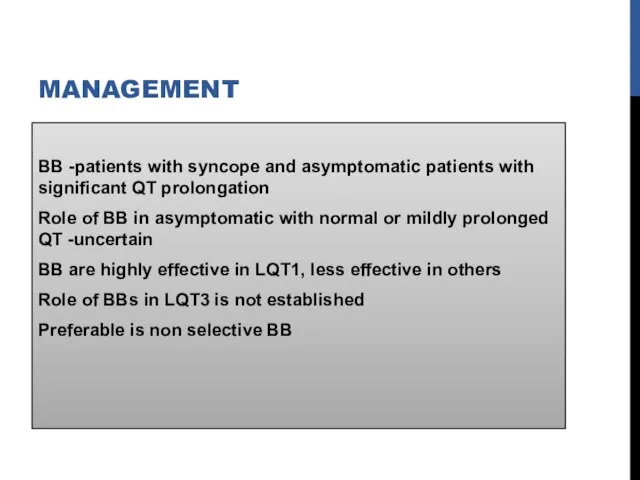
- 64. MANAGEMENT BB -patients with syncope and asymptomatic patients with significant QT prolongation Role of BB in
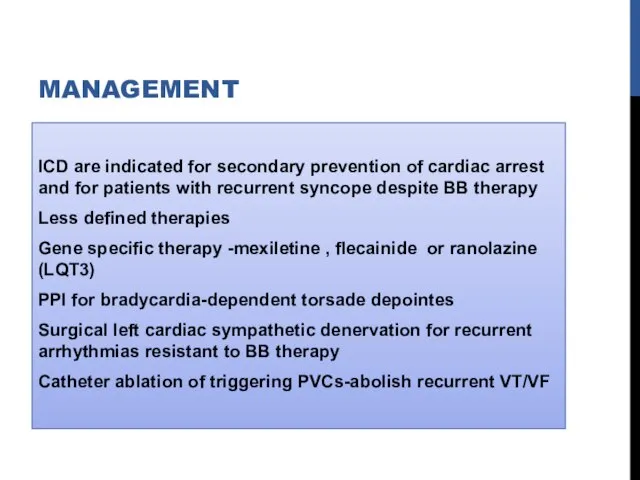
- 65. MANAGEMENT ICD are indicated for secondary prevention of cardiac arrest and for patients with recurrent syncope
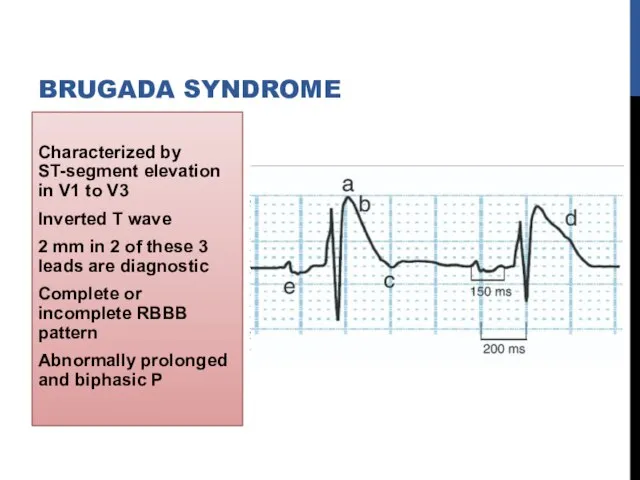
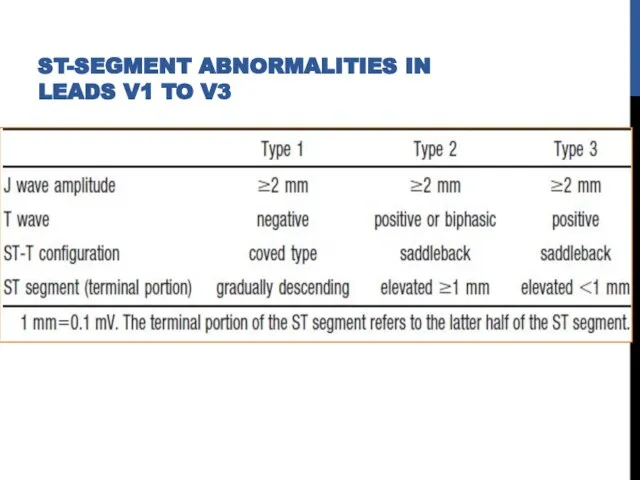
- 66. Characterized by ST-segment elevation in V1 to V3 Inverted T wave 2 mm in 2 of
- 67. ST-SEGMENT ABNORMALITIES IN LEADS V1 TO V3
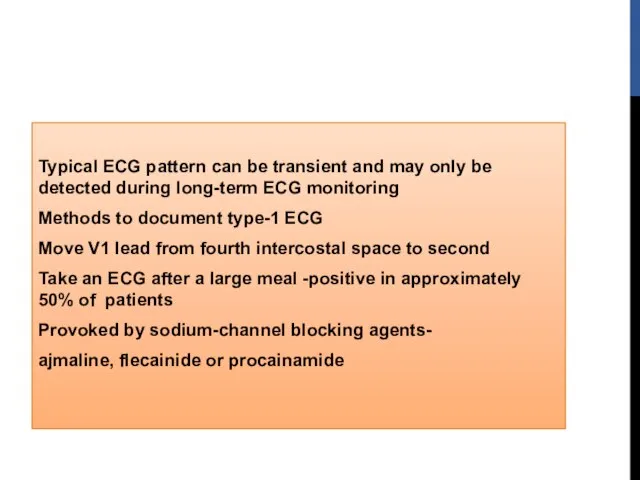
- 68. Typical ECG pattern can be transient and may only be detected during long-term ECG monitoring Methods
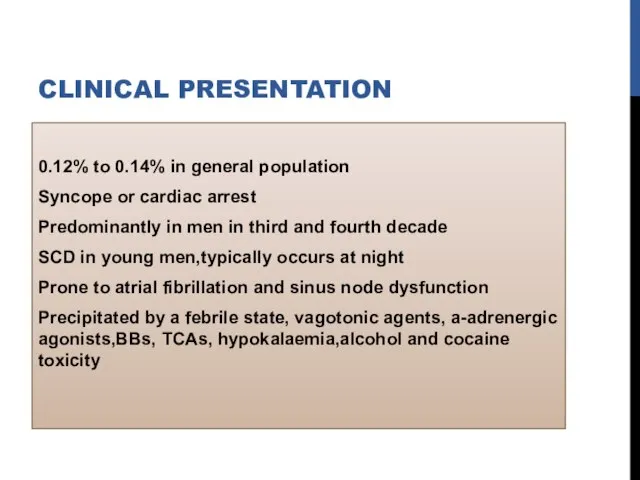
- 69. CLINICAL PRESENTATION 0.12% to 0.14% in general population Syncope or cardiac arrest Predominantly in men in
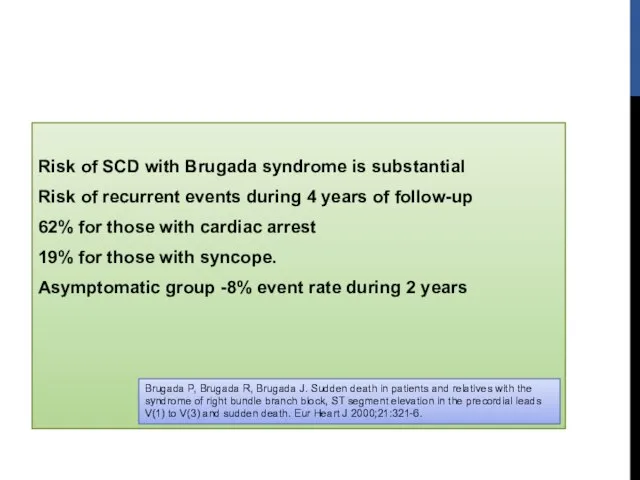
- 70. Risk of SCD with Brugada syndrome is substantial Risk of recurrent events during 4 years of
- 71. TREATMENT Drugs inhibit Ito (such as quinidine) and increase calcium current (such as isoproterenol) are effective
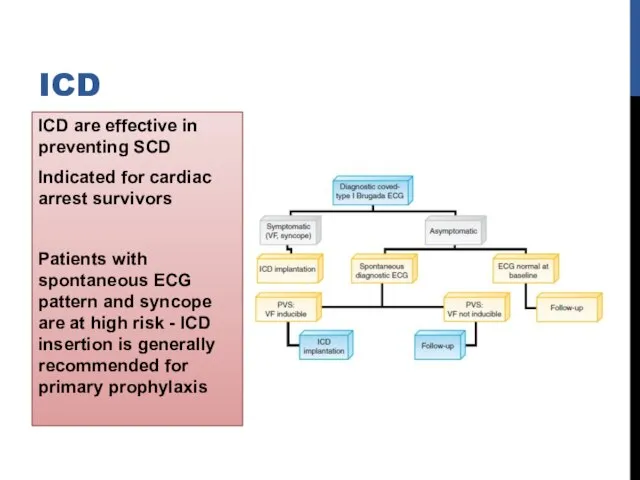
- 72. ICD are effective in preventing SCD Indicated for cardiac arrest survivors Patients with spontaneous ECG pattern
- 73. Different genes involved SCN5A gene mutations (BrS1) - loss of function of cardiac sodium channel (NaV
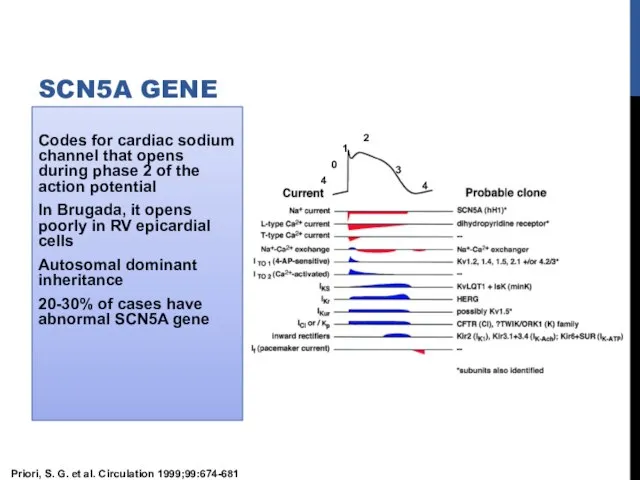
- 74. Codes for cardiac sodium channel that opens during phase 2 of the action potential In Brugada,
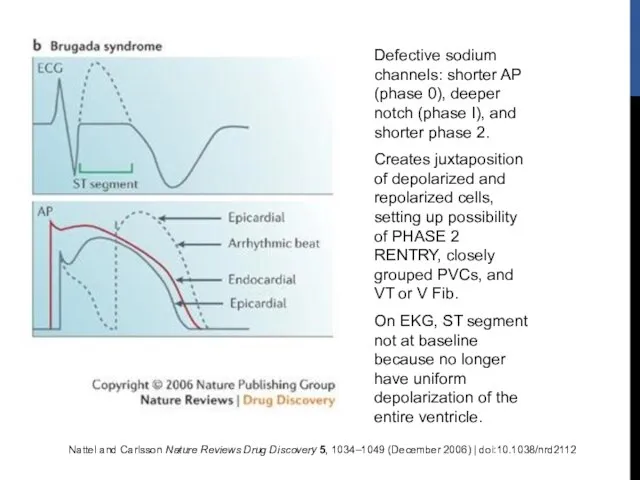
- 75. Nattel and Carlsson Nature Reviews Drug Discovery 5, 1034–1049 (December 2006) | doi:10.1038/nrd2112 Defective sodium channels:
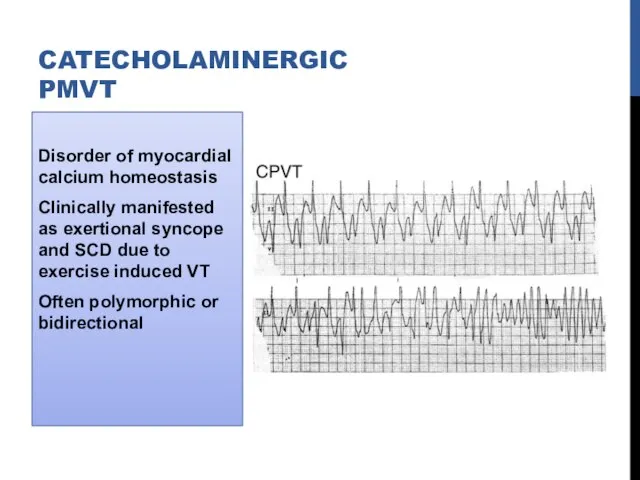
- 76. Disorder of myocardial calcium homeostasis Clinically manifested as exertional syncope and SCD due to exercise induced
- 77. Autosomal dominant (50% )-mutation of cardiac ryanodine receptor (RyR2 gene) Autosomal recessive (3% to 5% )-mutations
- 78. Ryanodine receptor spans membrane of sarcoplasmic reticulum Releases calcium triggered by calcium entry into cell through
- 79. Resting ECG is unremarkable, prominent U waves may be seen Typical VT patterns are reproducible with
- 80. Medical management-BB 46% may have recurrent events while receiving therapy CCB -limited effectiveness Flecainide (blocks RyR2
- 81. ICD Cardiac arrest Life-threatening VA despite maximal medical therapy Initial ICD shock with its accompanying pain
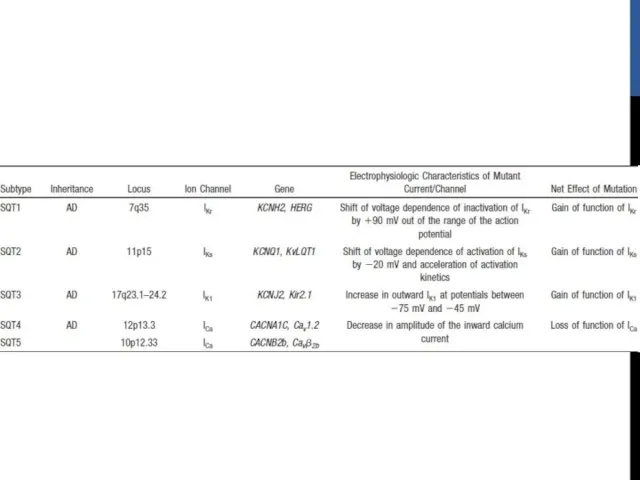
- 82. SHORT QT SYNDROME Rare disorder Characterized by short QT intervals of 300 to 320 ms Shortening
- 84. ICD implantation for secondary and primary prevention Preliminary observations suggest quinidine might be useful
- 85. IDIOPATHIC PROPRANOLOL-SENSITIVE VT (IPVT) Usually occurs by fifth decade of life Can arise from LV or
- 86. TREATMENT OF IPVT BBs effective in acute situations Insufficient information available regarding long-term management Survivors of
- 89. REFERENCES ZIPES 5th EDITION BRAUNWALD 9TH EDITION HURST 13TH EDITION VENTRICULAR ARRHYTHMIAS IN NORMAL HEARTS,SHUAIB LATIF,
- 91. Скачать презентацию

 Көздің торлы қабығының көктамыр тромбоз
Көздің торлы қабығының көктамыр тромбоз Кровотечение. Классификация по локализации излившейся крови, по характеру поврежденных сосудов, по скорости истечения
Кровотечение. Классификация по локализации излившейся крови, по характеру поврежденных сосудов, по скорости истечения Toshkent davlat stomatalogiya instituti yuz-jag’ kasalliklari va jarohatlari
Toshkent davlat stomatalogiya instituti yuz-jag’ kasalliklari va jarohatlari Фармакология
Фармакология Особенности нервно-психического развития детей первого года жизни
Особенности нервно-психического развития детей первого года жизни Прионные инфекции
Прионные инфекции Лабораторное исследование мокроты (лекция 1)
Лабораторное исследование мокроты (лекция 1) Поллиноз. Проявления поллиноза
Поллиноз. Проявления поллиноза Инфекции передаваемые половым путём
Инфекции передаваемые половым путём Респираторлы дисстресс синдромы
Респираторлы дисстресс синдромы Заболевания сердечно-сосудистой системы
Заболевания сердечно-сосудистой системы Арсеникум альбум (Яд). Общее действие
Арсеникум альбум (Яд). Общее действие Тыныс алу жолдарының бактериалды инфекциясының қоздырғышы - стафилококктар, стрептококктар
Тыныс алу жолдарының бактериалды инфекциясының қоздырғышы - стафилококктар, стрептококктар Нарушения ритма и проводимости
Нарушения ритма и проводимости Определение вида осанки в зависимости от степени выраженности изгибов позвоночника. Антропометрия. Типы телосложения
Определение вида осанки в зависимости от степени выраженности изгибов позвоночника. Антропометрия. Типы телосложения Что я знаю о своей профессии?
Что я знаю о своей профессии? Патология пуповины
Патология пуповины Современные технологии организации предрейсовых (послерейсовых) медицинских осмотров и управления корпоративным здоровьем
Современные технологии организации предрейсовых (послерейсовых) медицинских осмотров и управления корпоративным здоровьем Оказание первой помощи спортсменам в условиях тренировок и соревнований
Оказание первой помощи спортсменам в условиях тренировок и соревнований Клинически узкий таз. Крупный плод
Клинически узкий таз. Крупный плод Брюшной тиф. Шигеллёз. Сестринское дело
Брюшной тиф. Шигеллёз. Сестринское дело Седативные лекарственные средства
Седативные лекарственные средства Количественная оценка факторов риска развития заболевания
Количественная оценка факторов риска развития заболевания Правила использования медицинских масок
Правила использования медицинских масок Кенеттен өлім
Кенеттен өлім Гигиена голоса. Проблемы голосовых связок у вокалистов
Гигиена голоса. Проблемы голосовых связок у вокалистов Биоэтика и реализация соматических прав в странах Арабского мира
Биоэтика и реализация соматических прав в странах Арабского мира Границы сердца. Проекция клапанов сердца
Границы сердца. Проекция клапанов сердца