Содержание
- 3. Liver cirrhosis is a chronic liver disease accompanied by irreversible replacement of parenchymal liver tissue by
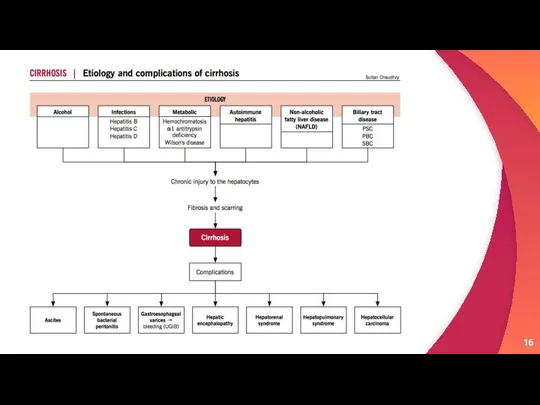
- 4. Etiology Alcohol Hepatitis B can cause liver inflammation and damage that can lead to cirrhosis. Hepatitis
- 5. Damage to the bile ducts, which function to drain bile: One example of such a condition
- 6. Classification 1
- 7. According to etiology: Postinfectious cirrhosis- viruses, parasites, syphilis, bacterial infection of biliary tract Toxic and toxic
- 8. According to macroscopic appearance: Micronodular cirrhosis Macronodular cirrhosis According to microscopic appearance: Monolobular cirrhosis Multilobular cirrhosis
- 9. According to course: Active Inactive
- 10. Pathogenesis 2
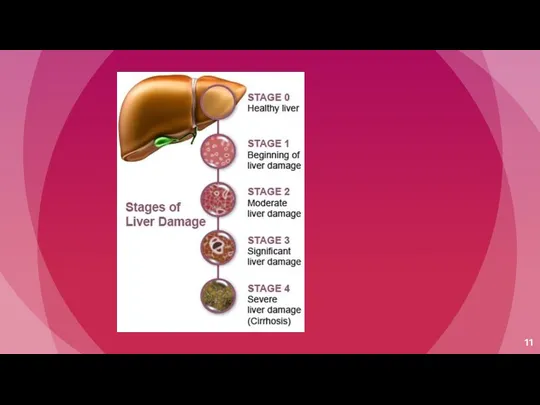
- 12. Irrespective of the aetiology, cirrhosis in general is initiated by hepatocellular necrosis Replacement of BM collagen
- 13. ECM regulates cellular activity and availability of growth factors Decorin and biglycan binds TGF-B Fibronectin and
- 14. HSC activation represents a critical event in the fibrosis This cell become the primary source of
- 15. Sources of ECM HSC Bone marrow derive cells Epithelial mesenchymal transition Portal fibroblast
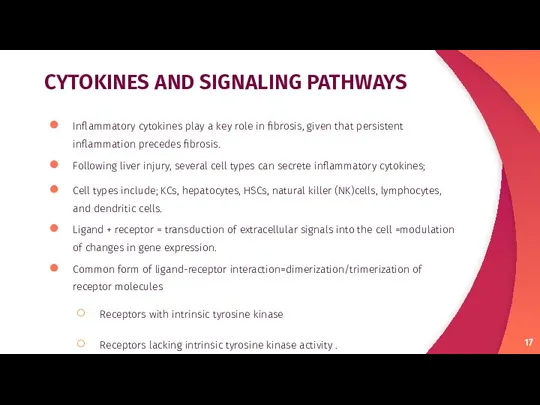
- 17. CYTOKINES AND SIGNALING PATHWAYS Inflammatory cytokines play a key role in fibrosis, given that persistent inflammation
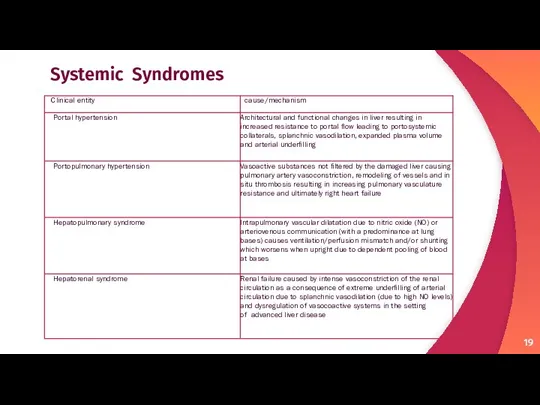
- 19. Systemic Syndromes
- 20. Clinical Features 3
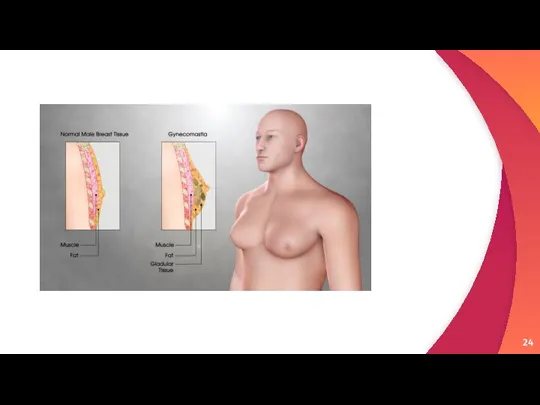
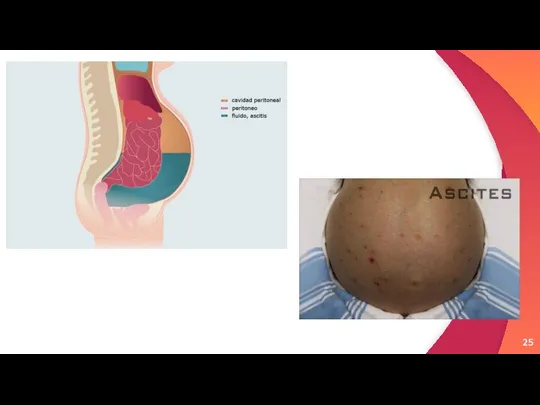
- 21. More serious symptoms include: confusion and difficulty thinking clearly abdominal swelling (ascites) swelling of the legs
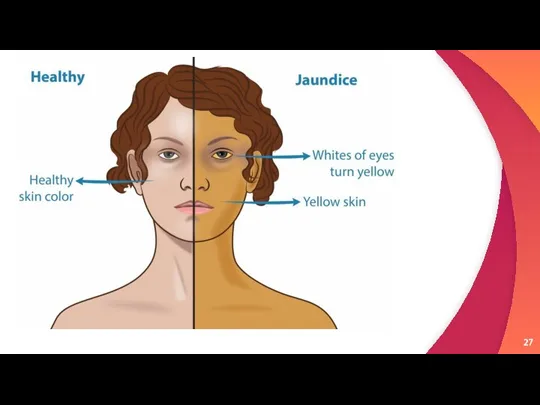
- 22. Liver dysfunction The following features are a direct consequence of liver cells not functioning. Spider angiomata
- 23. Spider angiomata Palmnar Erythema
- 26. Epitaxis Jaundice
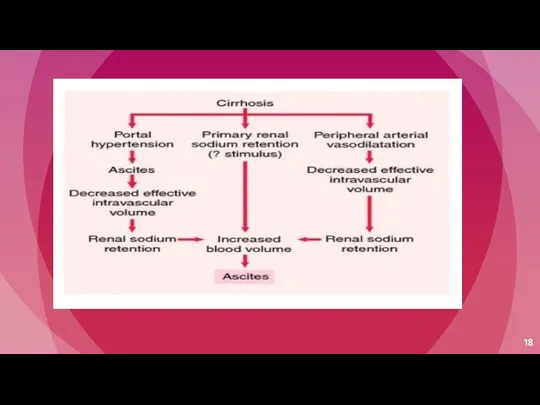
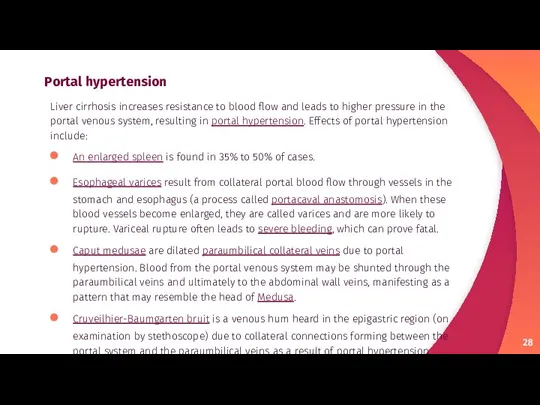
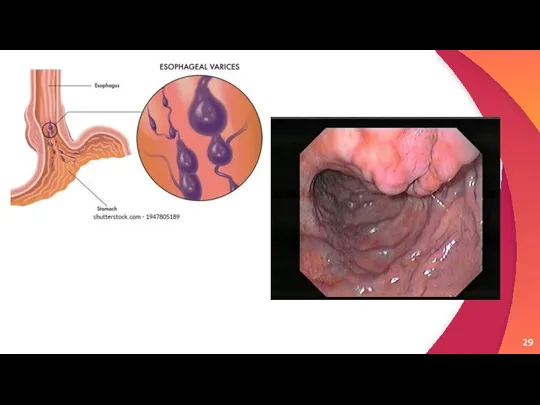
- 28. Portal hypertension Liver cirrhosis increases resistance to blood flow and leads to higher pressure in the
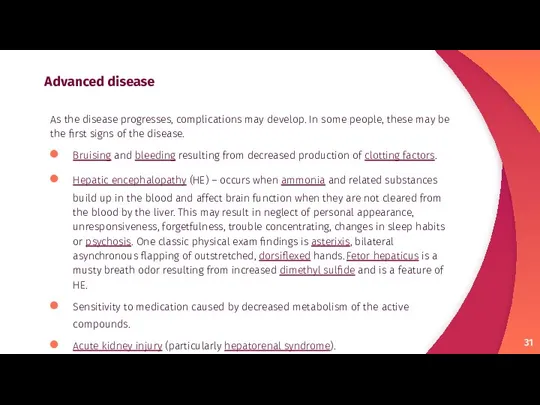
- 31. Advanced disease As the disease progresses, complications may develop. In some people, these may be the
- 32. Bruising Cachexic patient with jaundice
- 33. Lab findings The following findings are typical in cirrhosis: Thrombocytopenia – typically multifactorial. Due to alcoholic
- 34. Prothrombin time – increases, since the liver synthesizes clotting factors. Globulins – increased due to shunting
- 35. Other laboratory studies performed in newly diagnosed cirrhosis may include: Serology for hepatitis viruses, autoantibodies (ANA,
- 36. Liver ultrasound to assess the severity of cirrhosis. Liver biopsy to identify liver cell changes &
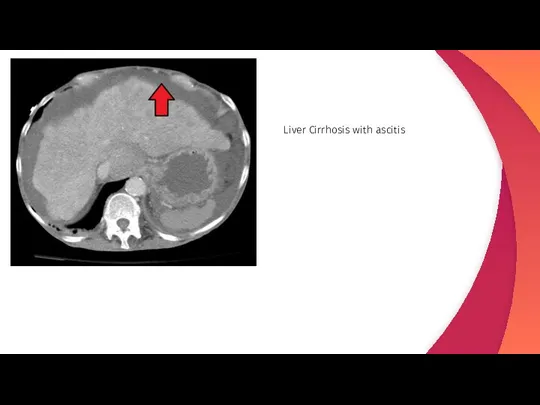
- 37. Liver Cirrhosis with ascitis
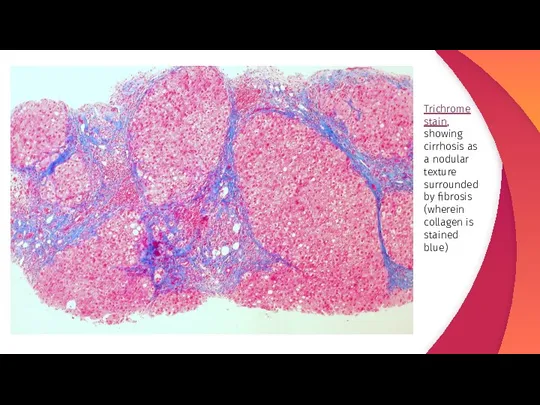
- 38. Trichrome stain, showing cirrhosis as a nodular texture surrounded by fibrosis (wherein collagen is stained blue)
- 39. Treatment & Prevention 3
- 40. Treatment for cirrhosis varies based on what caused it and how far the disorder has progressed.
- 41. Practicing sex with a barrier method can reduce the risk of getting hepatitis B or C.
- 43. Скачать презентацию





 Противоопухолевые антибиотики. Классификация
Противоопухолевые антибиотики. Классификация LPG-массаж
LPG-массаж Фенилкетонурия
Фенилкетонурия Третичный период сифилиса
Третичный период сифилиса Алгоритм действия медсестры при почечной колике
Алгоритм действия медсестры при почечной колике Врачебно – педагогический контроль, самоконтроль при занятиях физической культурой и спортом
Врачебно – педагогический контроль, самоконтроль при занятиях физической культурой и спортом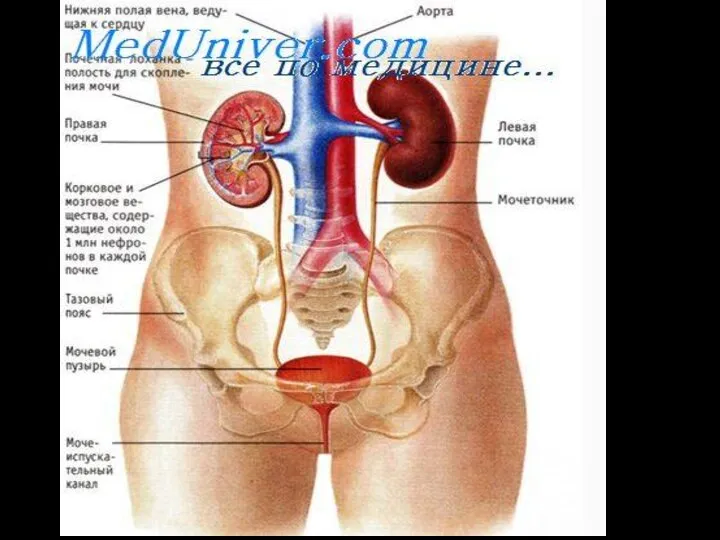 Мочевыделительная система
Мочевыделительная система ҚР және РФ Пародонтит бойынша протоколдардың салыстырмалы диагностикасы
ҚР және РФ Пародонтит бойынша протоколдардың салыстырмалы диагностикасы Применение лазера в медицине
Применение лазера в медицине Анализ формы тела и линий внешности: коррекция осанки
Анализ формы тела и линий внешности: коррекция осанки Балардағы мезаденит
Балардағы мезаденит Нефроптоз
Нефроптоз Индивидуальный подбор при расстройствах регуляции РС. Лекция 16
Индивидуальный подбор при расстройствах регуляции РС. Лекция 16 Қан тамырлар жүйесі. Жүрек құрылысы
Қан тамырлар жүйесі. Жүрек құрылысы Инновационные технологии в медицинской оптике
Инновационные технологии в медицинской оптике Патология обмена веществ
Патология обмена веществ Экстремальные состояния
Экстремальные состояния № 2299 ж/е №526 бұйрықтары
№ 2299 ж/е №526 бұйрықтары Отчет по воронке продаж
Отчет по воронке продаж Нейросифилис. Сифилис
Нейросифилис. Сифилис Ежедневная гигиена, купание больного в ванной, подмывание женщин и мужчин, мытье подопечного в кровати
Ежедневная гигиена, купание больного в ванной, подмывание женщин и мужчин, мытье подопечного в кровати Должностные обязанности и права младшего медперсонала отделения, объем работы, ее характеристика
Должностные обязанности и права младшего медперсонала отделения, объем работы, ее характеристика Различие психики животных и человека
Различие психики животных и человека Здоровье без лекарств. Естественная стимуляция защитных систем организма
Здоровье без лекарств. Естественная стимуляция защитных систем организма Коронавирус. Вакцинация
Коронавирус. Вакцинация Бронхиальная астма
Бронхиальная астма История болезни
История болезни Питание беременных
Питание беременных