Содержание
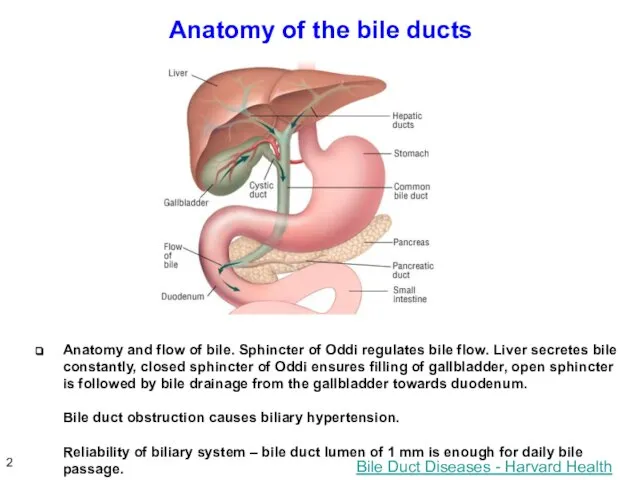
- 2. Anatomy of the bile ducts Bile Duct Diseases - Harvard Health Anatomy and flow of bile.
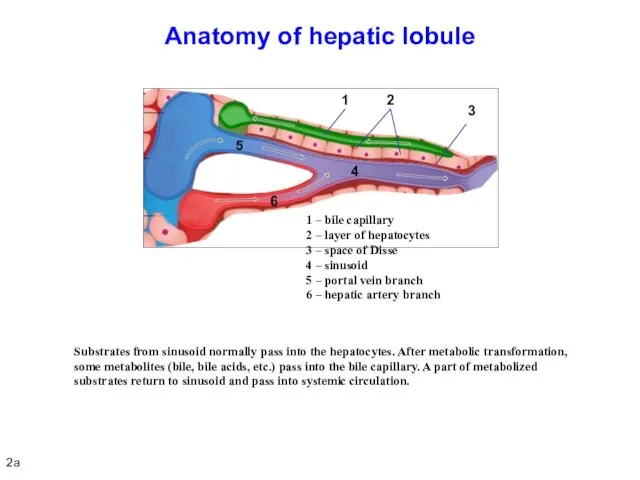
- 3. Anatomy of hepatic lobule Substrates from sinusoid normally pass into the hepatocytes. After metabolic transformation, some
- 4. Definition: any impairment of secretion and release of bile from the hepatocyte to the major duodenal
- 5. Cholemia Homeostasis disorders: vascular dilatation, reduced peripheral vascular resistance and total blood volume, bradycardia, vagal effects,
- 6. Painful and painless obstructive jaundice Various rates of biliary hypertension development (fast, sudden or slow, gradual)
- 7. PAINFUL OBSTRUCTIVE JAUNDICE 5
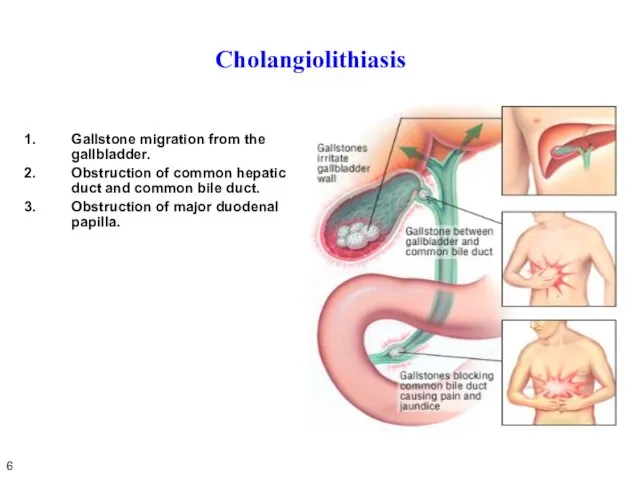
- 8. Cholangiolithiasis Gallstone migration from the gallbladder. Obstruction of common hepatic duct and common bile duct. Obstruction
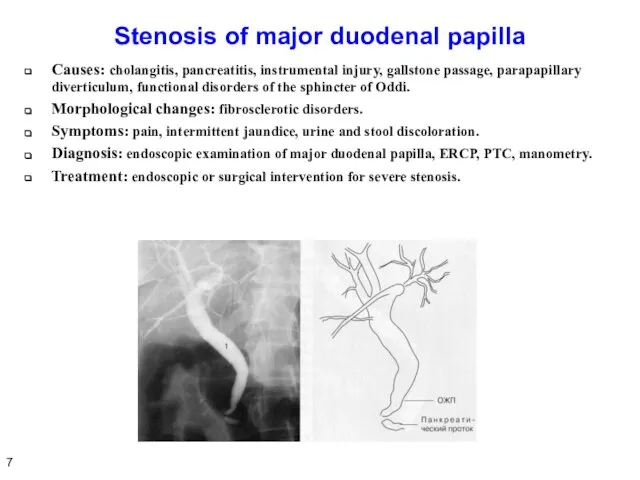
- 9. Stenosis of major duodenal papilla Causes: cholangitis, pancreatitis, instrumental injury, gallstone passage, parapapillary diverticulum, functional disorders
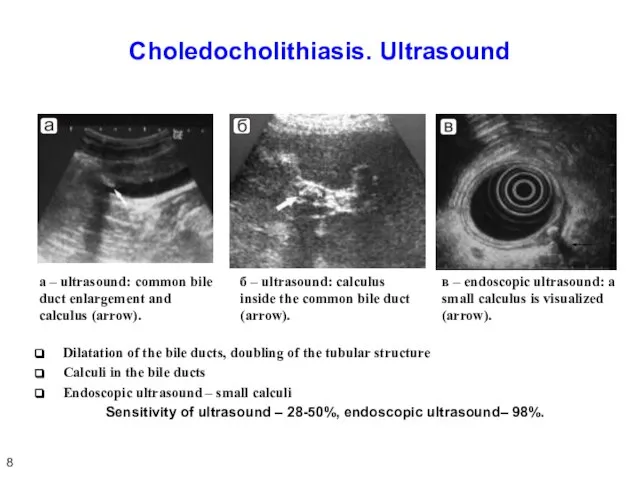
- 10. Choledocholithiasis. Ultrasound Dilatation of the bile ducts, doubling of the tubular structure Calculi in the bile
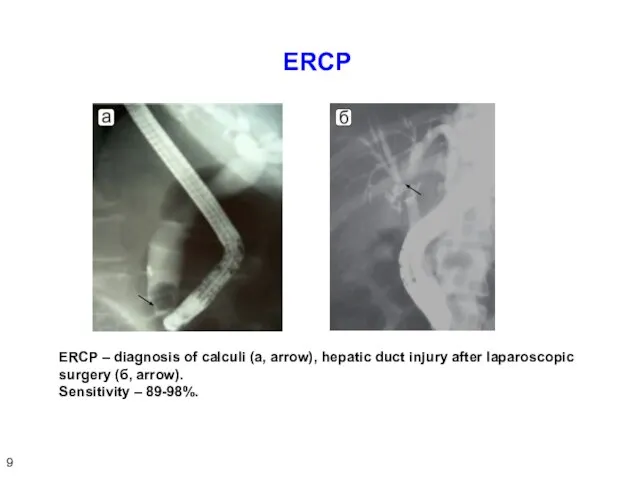
- 11. ERCP ERCP – diagnosis of calculi (а, arrow), hepatic duct injury after laparoscopic surgery (б, arrow).
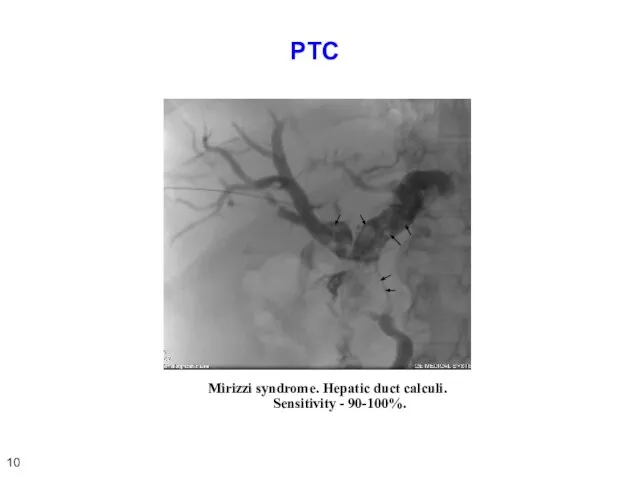
- 12. PTC Mirizzi syndrome. Hepatic duct calculi. Sensitivity - 90-100%. 10
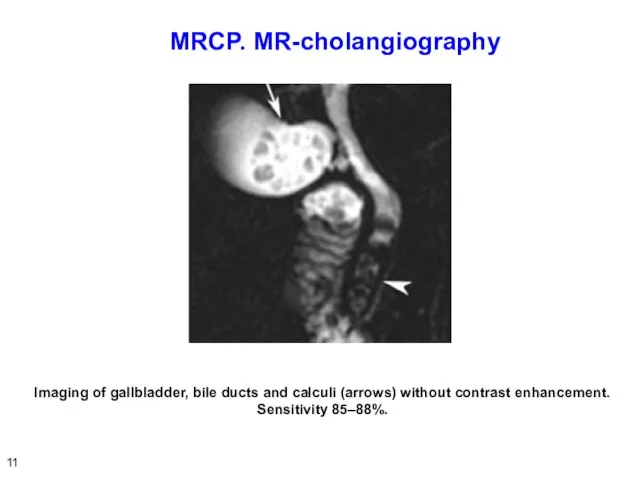
- 13. MRCP. МR-cholangiography Imaging of gallbladder, bile ducts and calculi (arrows) without contrast enhancement. Sensitivity 85–88%. 11
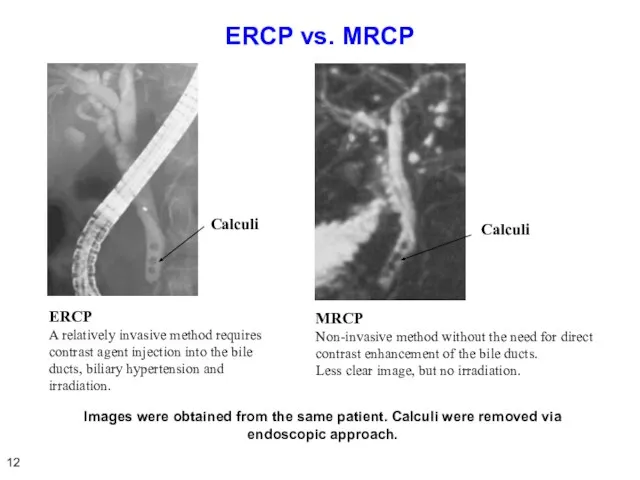
- 14. ERCP vs. MRCP ERCP A relatively invasive method requires contrast agent injection into the bile ducts,
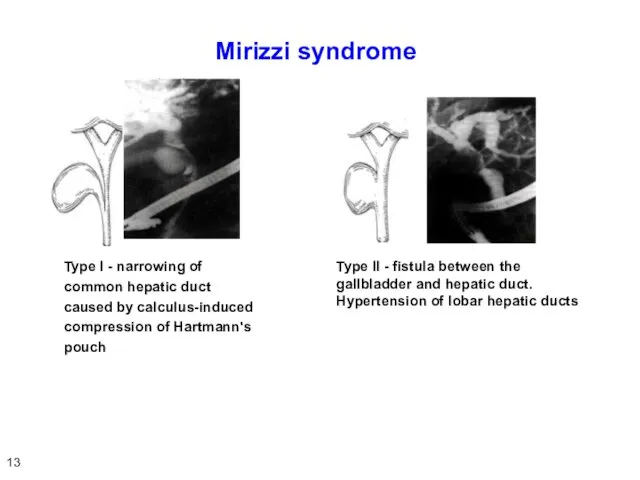
- 15. Mirizzi syndrome Type I - narrowing of common hepatic duct caused by calculus-induced compression of Hartmann's
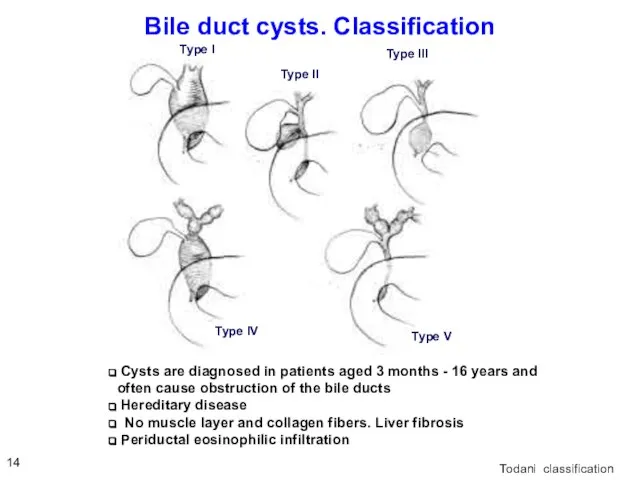
- 16. Bile duct cysts. Classification Todani classification Cysts are diagnosed in patients aged 3 months - 16
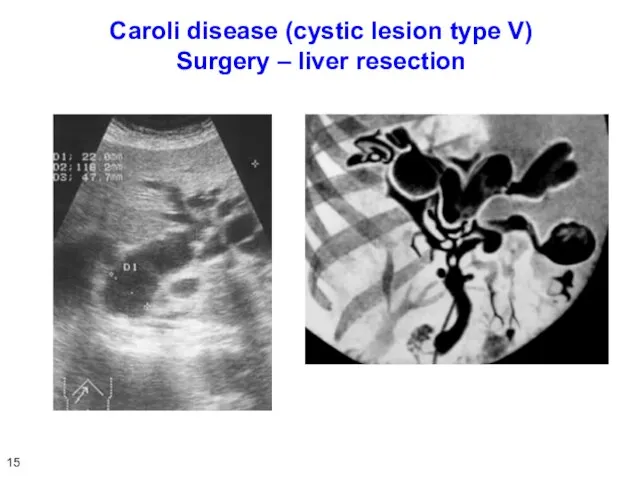
- 17. Caroli disease (cystic lesion type V) Surgery – liver resection 15
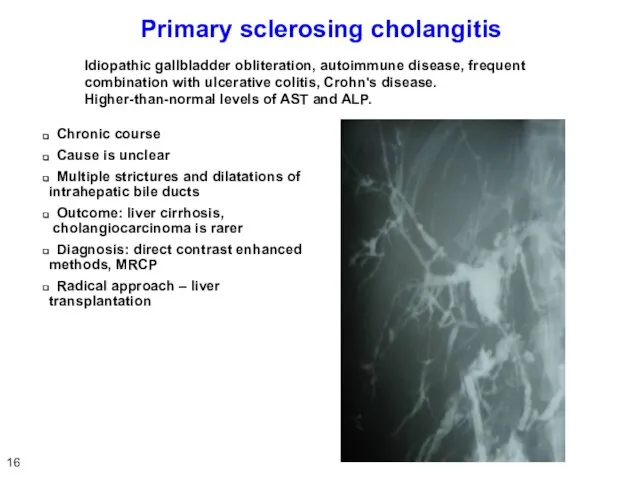
- 18. Primary sclerosing cholangitis Chronic course Cause is unclear Multiple strictures and dilatations of intrahepatic bile ducts
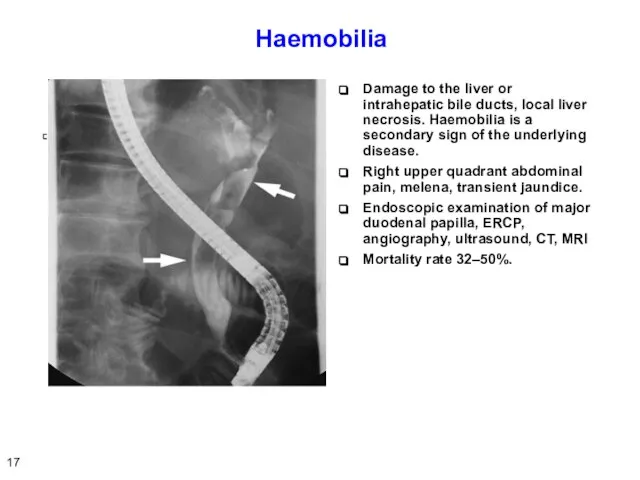
- 19. Haemobilia Damage to the liver or intrahepatic bile ducts, local liver necrosis. Haemobilia is a secondary
- 20. Parasitic invasion Opisthorchiasis (Ob, Volga basin, East Asia) Echinococcosis, alveococcosis, ascariasis, Fascioliasis– Fasciola gigantica Schistosomiasis –
- 21. Symptoms and diagnosis of painful obstructive jaundice Acute onset Scleral icterus Pain attack Dark urine, stool
- 22. ACUTE CHOLANGITIS 20
- 23. Acute cholangitis (AC) AC is an infectious inflammation of the bile ducts. Most often, AC develops
- 24. Cholangiovenous reflux Corrosion casting. Scanning electron microscopy Secretory pressure. Microbial metabolite pressure. L., Pellegrini C.A., Way
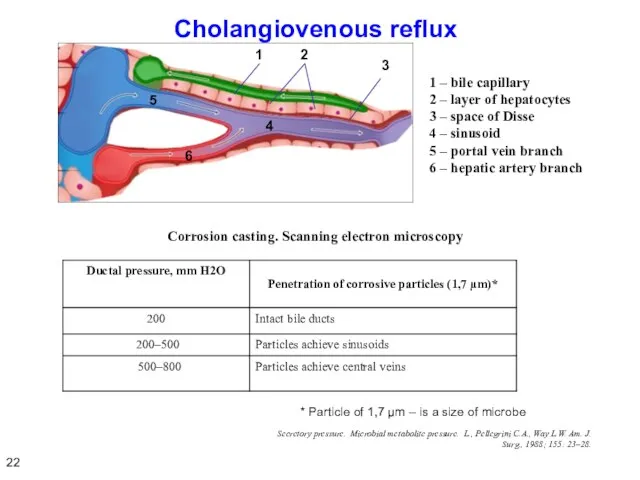
- 25. Symptoms of acute cholangitis Chills, fever Leukocytosis Infection Symptoms associated with biliary hypertension and obstructive jaundice
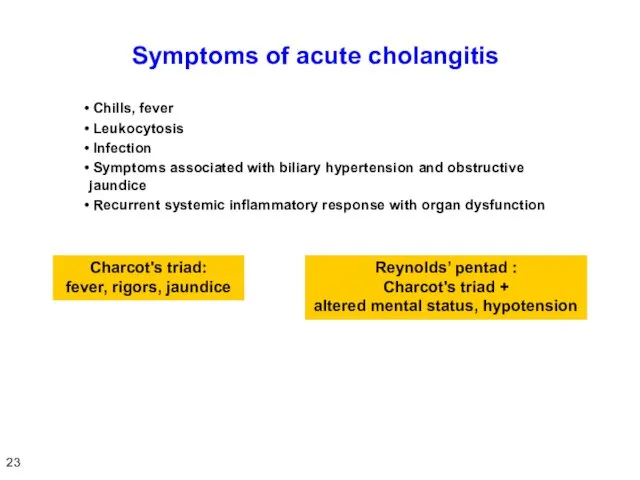
- 26. Causes of short-term SIRS and symptoms of sepsis Two factors: Large purulent surface of gallbladder, direct
- 27. Criteria of SIRS and sepsis Body temperature > 38ºC or Heart rate > 90 beats per
- 28. Organ dysfunction criteria CVS – hypotension requiring dopamine support CNS – impaired consciousness Respiratory system –
- 29. Renal failure in acute cholangitis Kidney is a main organ secreting bile components – cholemic nephropathy.
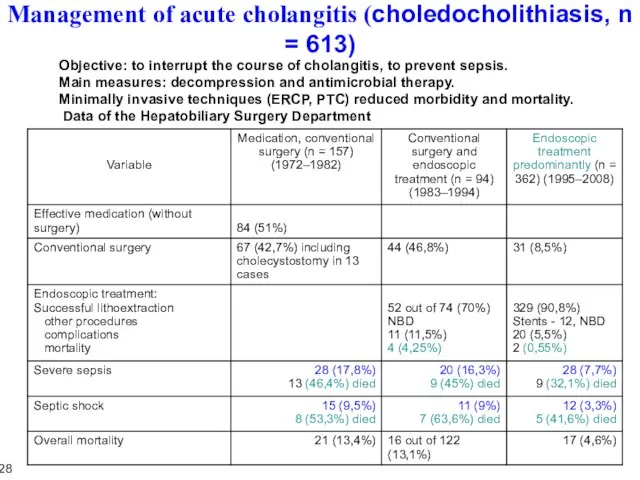
- 30. Management of acute cholangitis (choledocholithiasis, n = 613) Objective: to interrupt the course of cholangitis, to
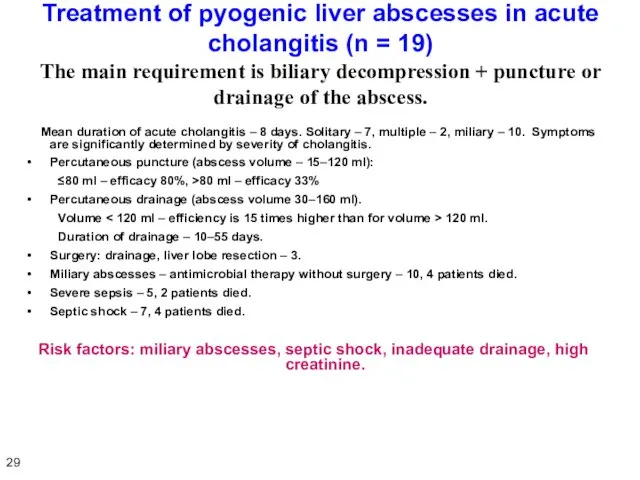
- 31. Treatment of pyogenic liver abscesses in acute cholangitis (n = 19) The main requirement is biliary
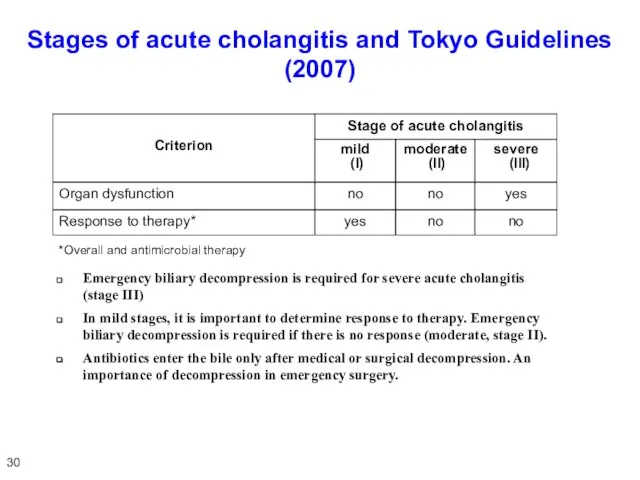
- 32. Stages of acute cholangitis and Tokyo Guidelines (2007) *Overall and antimicrobial therapy Emergency biliary decompression is
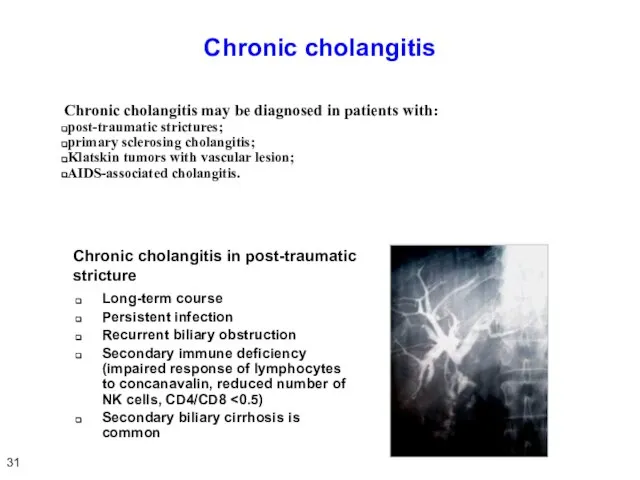
- 33. Chronic cholangitis Chronic cholangitis may be diagnosed in patients with: post-traumatic strictures; primary sclerosing cholangitis; Klatskin
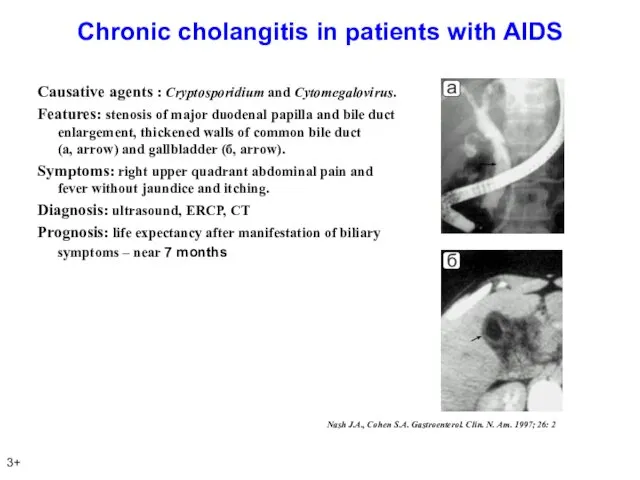
- 34. Chronic cholangitis in patients with AIDS Causative agents : Cryptosporidium and Cytomegalovirus. Features: stenosis of major
- 35. Conclusion Acute cholangitis is characterized by purulent process proceeding on the background of cholemia and acholia
- 36. PAINLESS OBSTRUCTIVE JAUNDICE 35
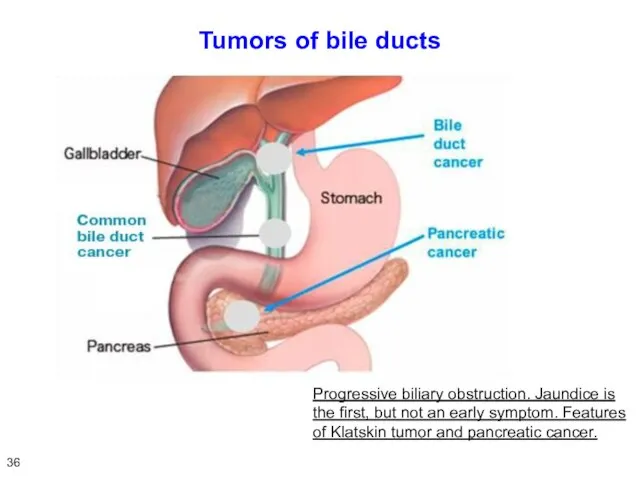
- 37. Tumors of bile ducts Progressive biliary obstruction. Jaundice is the first, but not an early symptom.
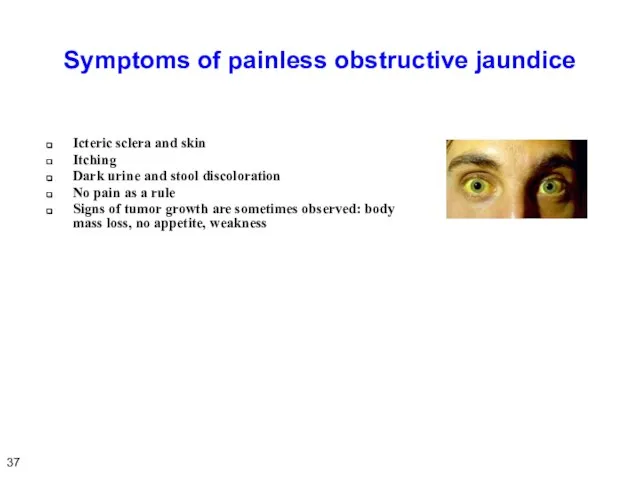
- 38. Symptoms of painless obstructive jaundice Icteric sclera and skin Itching Dark urine and stool discoloration No
- 39. Cancer of hepatic and common bile ducts Common hepatic duct (Klatskin tumor) 56% Common bile duct
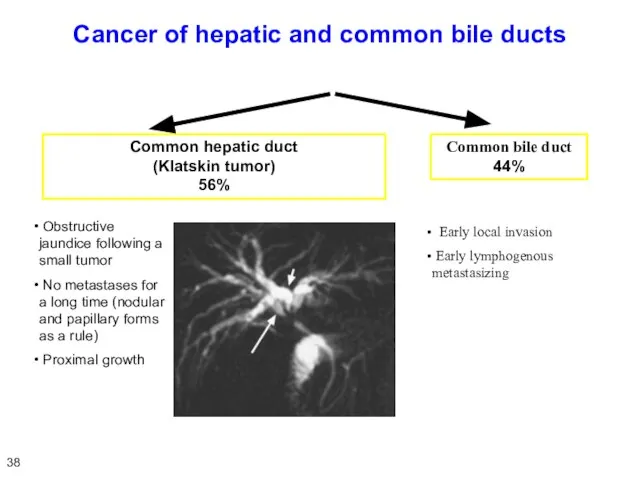
- 40. Classification of hepatic duct cancer (Bismuth) 39
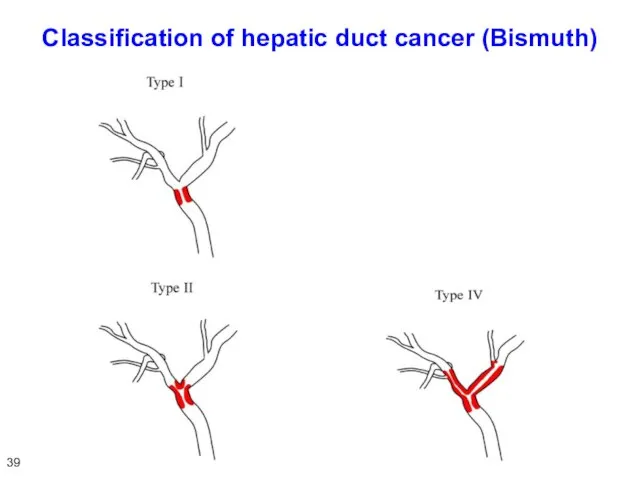
- 41. MR-cholangiography in Klatskin tumor 40
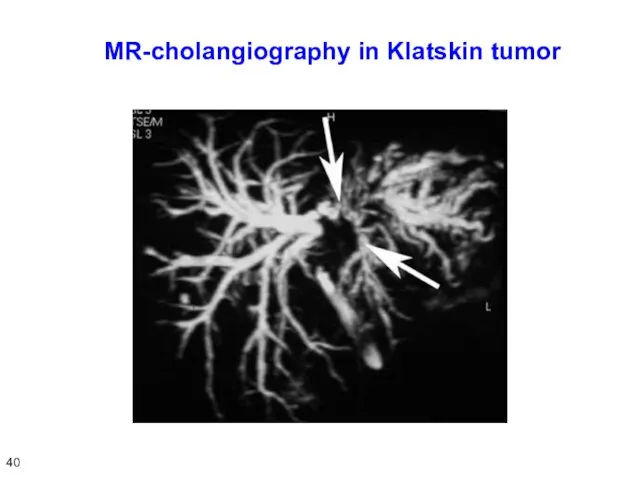
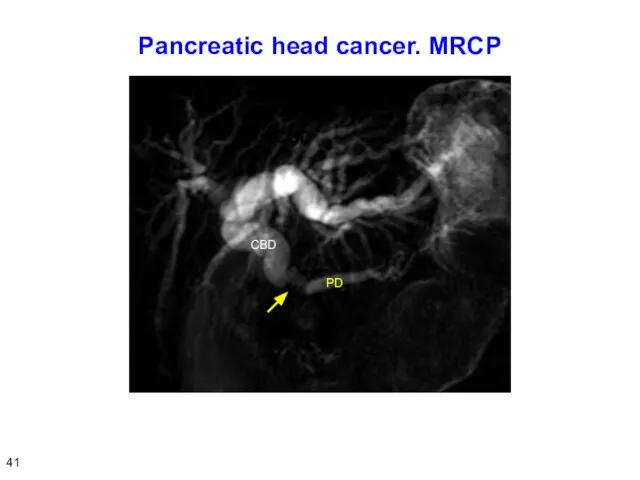
- 42. Pancreatic head cancer. MRCP 41
- 43. Differential diagnosis of obstructive and parenchymatous jaundice Patients with a painless obstructive jaundice do not notice
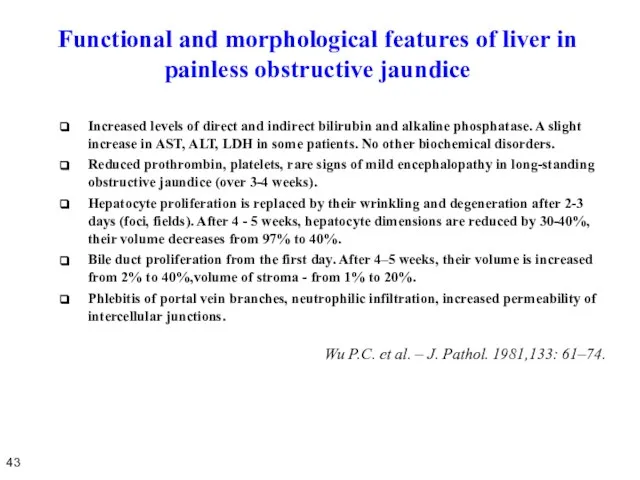
- 44. Functional and morphological features of liver in painless obstructive jaundice Increased levels of direct and indirect
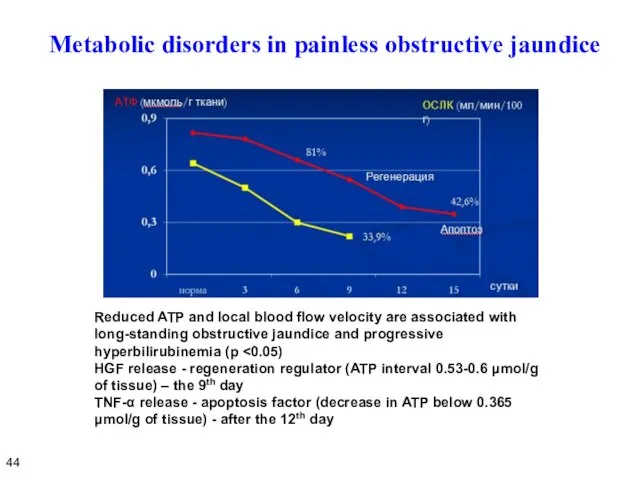
- 45. Metabolic disorders in painless obstructive jaundice Reduced ATP and local blood flow velocity are associated with
- 46. Conclusion on disorders arising in painless obstructive jaundice Painless obstructive jaundice causes severe functional and morphological
- 47. PREOPERATIVE DECOMPRESSION 46
- 48. Preoperative decompression of the bile ducts Methods of preoperative biliary decompression: Percutaneous cholangiostomy. Endoscopic nasobiliary drainage
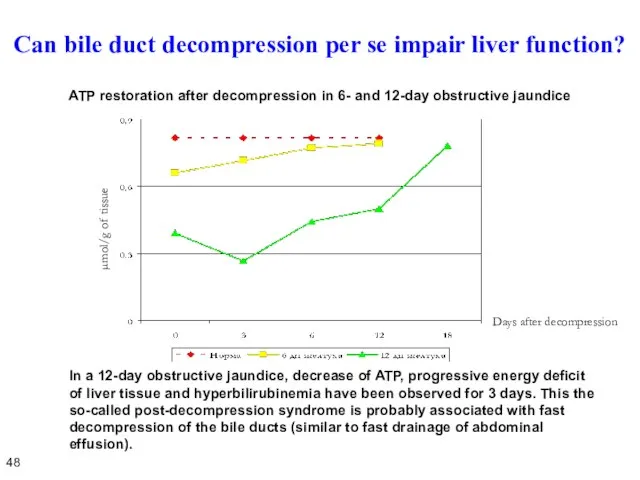
- 49. Can bile duct decompression per se impair liver function? In a 12-day obstructive jaundice, decrease of
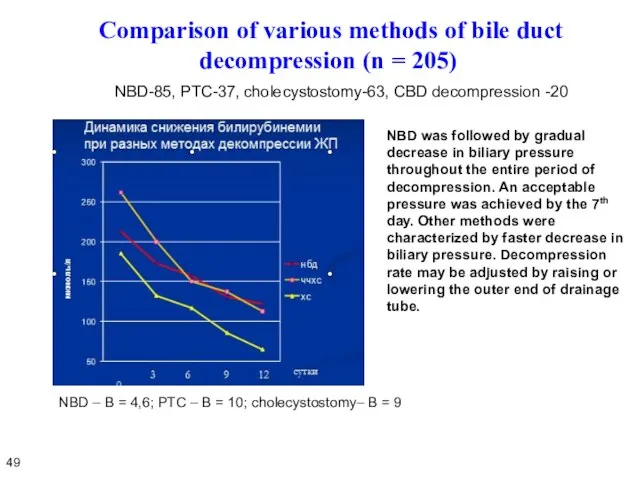
- 50. Comparison of various methods of bile duct decompression (n = 205) NBD-85, PTC-37, cholecystostomy-63, CBD decompression
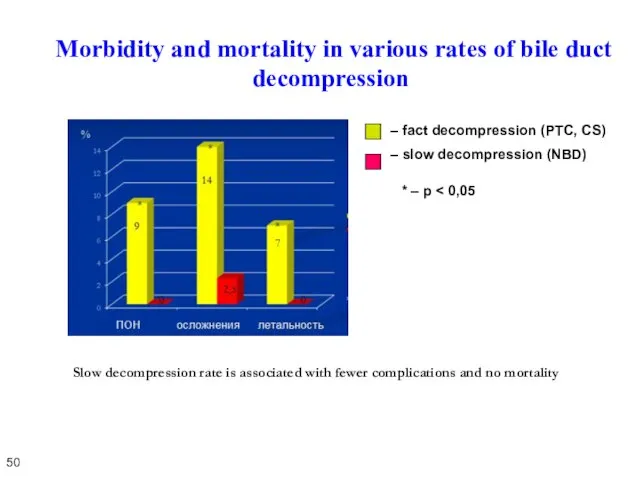
- 51. Morbidity and mortality in various rates of bile duct decompression * – p Slow decompression rate
- 52. Positive and negative aspects of preoperative biliary decompression 51 Opinions on stenting are still controversial. However,
- 53. Features of preoperative biliary decompression in Klatskin tumor 52 Radical surgery for Klatskin tumor implies extended
- 55. Скачать презентацию
 Врожденные аномалии у детей
Врожденные аномалии у детей Профилактика вирусно-бактериологической инфекции
Профилактика вирусно-бактериологической инфекции Основные функции мелатонина
Основные функции мелатонина Етіологія, патогенез, клініка, діагностика, профілактика та лікування сагітальних аномалій прикусу: медіального, дистального
Етіологія, патогенез, клініка, діагностика, профілактика та лікування сагітальних аномалій прикусу: медіального, дистального Частная психопатология
Частная психопатология Зубо-челюстно-лицевой комплекс тканей
Зубо-челюстно-лицевой комплекс тканей Результаты исследования кремов с антивозрастным эффектом
Результаты исследования кремов с антивозрастным эффектом О доступности медицинских услуг пациентам с ограниченными возможностями здоровья
О доступности медицинских услуг пациентам с ограниченными возможностями здоровья Вклад в развитие анатомии Леонардо да Винчи
Вклад в развитие анатомии Леонардо да Винчи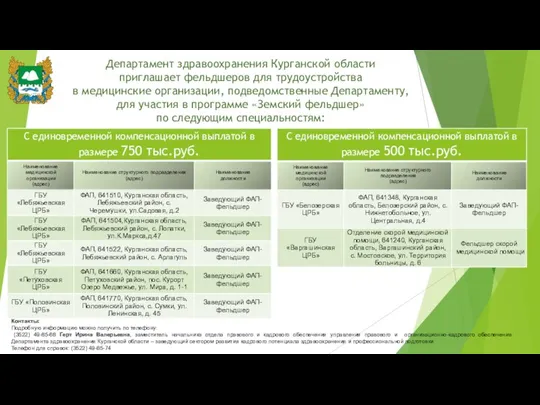 Программа Земский фельдшер
Программа Земский фельдшер Позитивная психотерапия
Позитивная психотерапия Физическое здоровье
Физическое здоровье Медицинская информатика
Медицинская информатика Патология пуповины
Патология пуповины Демодекоз
Демодекоз Преемственность и комплексный подход в оказании психиатрической помощи. IV Муратовские научные чтения
Преемственность и комплексный подход в оказании психиатрической помощи. IV Муратовские научные чтения Болезни, связанные с нехваткой химических элементов
Болезни, связанные с нехваткой химических элементов Семейство Vibrionaceae
Семейство Vibrionaceae СПИД и его профилактика
СПИД и его профилактика Тератома. Плод-паразит
Тератома. Плод-паразит Строение сердца человека, причины его заболеваний
Строение сердца человека, причины его заболеваний Методические рекомендации для руководителей медицинских организаций первичного звена здравоохранения
Методические рекомендации для руководителей медицинских организаций первичного звена здравоохранения Полипрагмазия. Анализ исследования о множественном приеме лекарств у пожилых
Полипрагмазия. Анализ исследования о множественном приеме лекарств у пожилых Мемристорный протез функционального отдела спинного мозга. Исследовательский проект
Мемристорный протез функционального отдела спинного мозга. Исследовательский проект Современные аспекты сестринского ухода при лейкозах
Современные аспекты сестринского ухода при лейкозах Здоровье не все, но все без здоровья ничто
Здоровье не все, но все без здоровья ничто ХСН. Клиника. Осмотр. Физикальные данные
ХСН. Клиника. Осмотр. Физикальные данные Влияние технологий подготовки к родам на уровень инфекций, связанных с оказанием медицинской помощи в послеродовом периоде
Влияние технологий подготовки к родам на уровень инфекций, связанных с оказанием медицинской помощи в послеродовом периоде