Слайд 2CIRRHOSIS
• End stage liver disease (irreversible)
• Result from many causes of chronic
liver disease:
• Viral Hepatitis (especially B and C)
• Alcoholic liver disease
• Non-alcoholic fatty liver disease
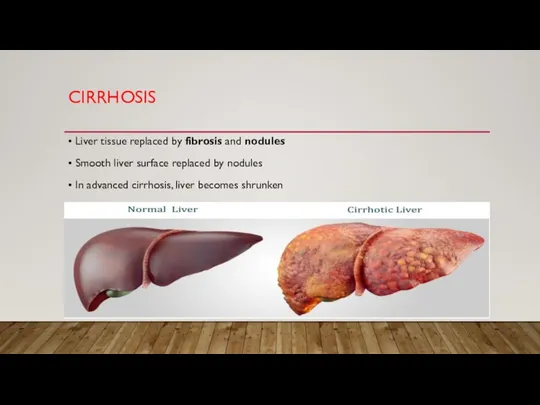
Слайд 3CIRRHOSIS
• Liver tissue replaced by fibrosis and nodules
• Smooth liver surface replaced
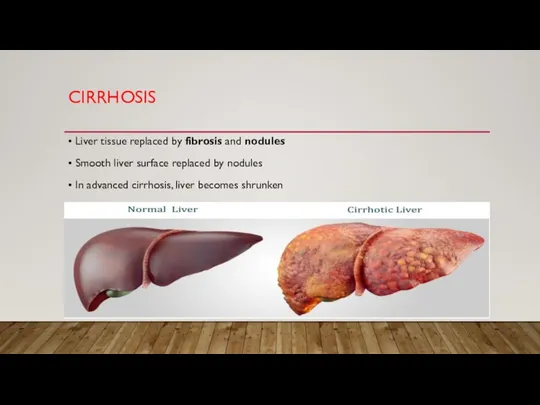
by nodules
• In advanced cirrhosis, liver becomes shrunken
Слайд 4CLINICAL FEATURES
• Hyperammonemia
• Asterixis, confusion, coma
Слайд 5HYPERAMMONEMIA
TREATMENT
• Low protein diet
• Lactulose
• Synthetic disaccharide (laxative)
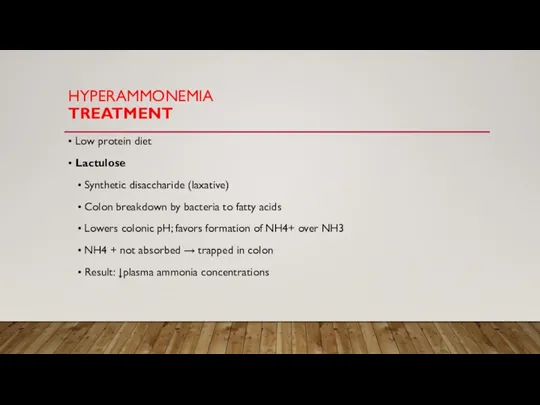
• Colon breakdown by bacteria to fatty acids
• Lowers colonic pH; favors formation of NH4+ over NH3
• NH4 + not absorbed → trapped in colon
• Result: ↓plasma ammonia concentrations
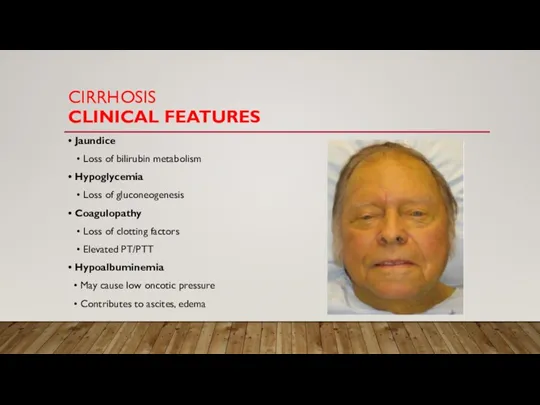
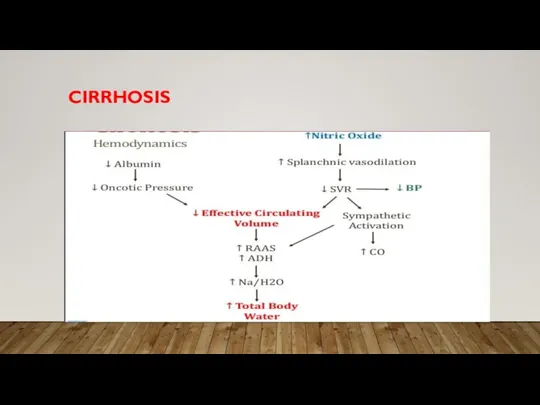
Слайд 6CIRRHOSIS
CLINICAL FEATURES
• Jaundice
• Loss of bilirubin metabolism
• Hypoglycemia
• Loss
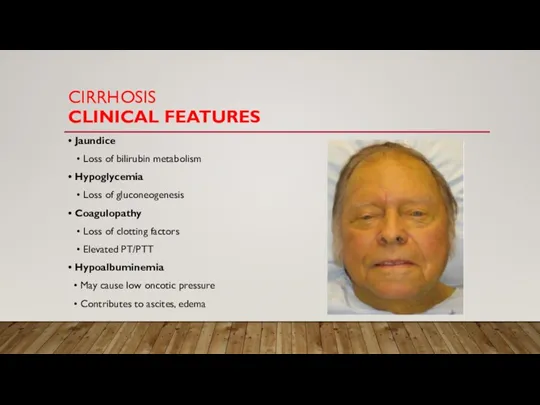
of gluconeogenesis
• Coagulopathy
• Loss of clotting factors
• Elevated PT/PTT
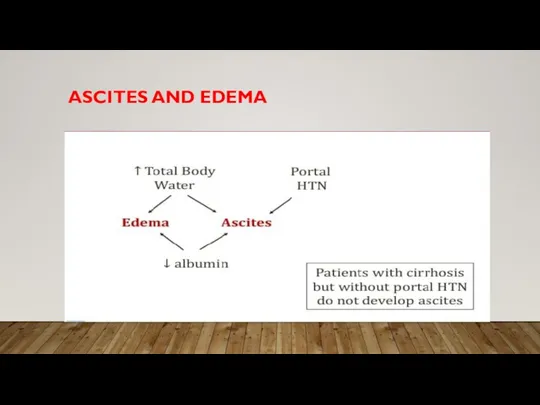
• Hypoalbuminemia
• May cause low oncotic pressure
• Contributes to ascites, edema
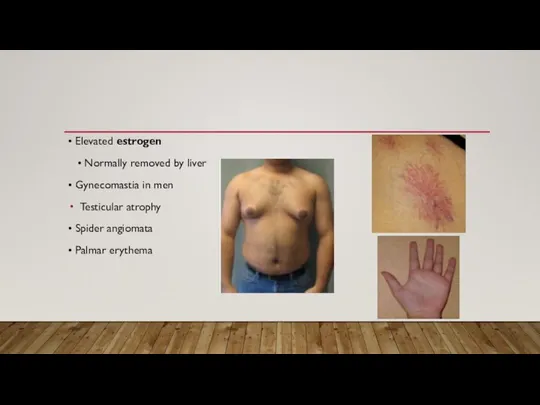
Слайд 7• Elevated estrogen
• Normally removed by liver
• Gynecomastia in
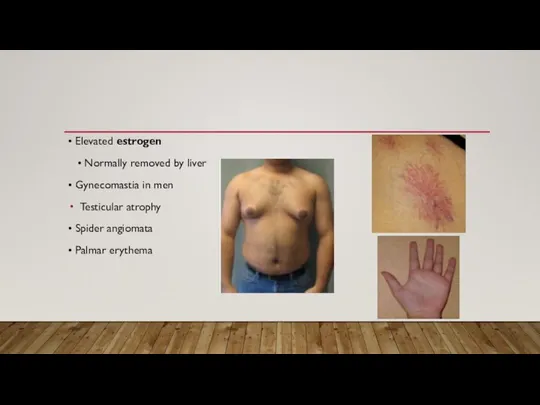
men
Testicular atrophy
• Spider angiomata
• Palmar erythema
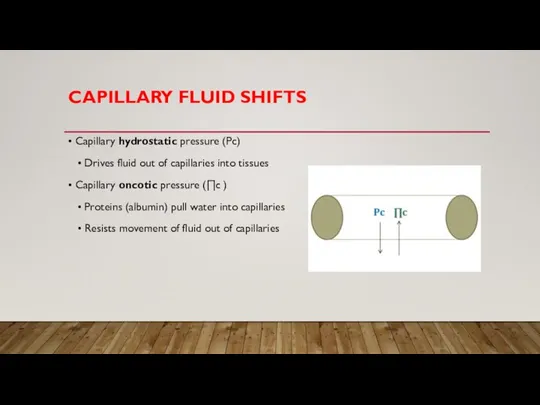
Слайд 8CAPILLARY FLUID SHIFTS
• Capillary hydrostatic pressure (Pc)
• Drives fluid out of
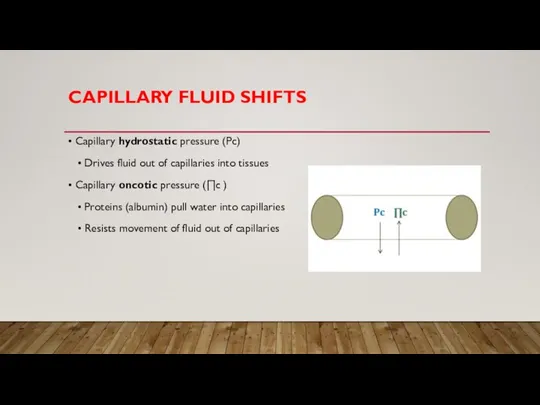
capillaries into tissues
• Capillary oncotic pressure (∏c )
• Proteins (albumin) pull water into capillaries
• Resists movement of fluid out of capillaries
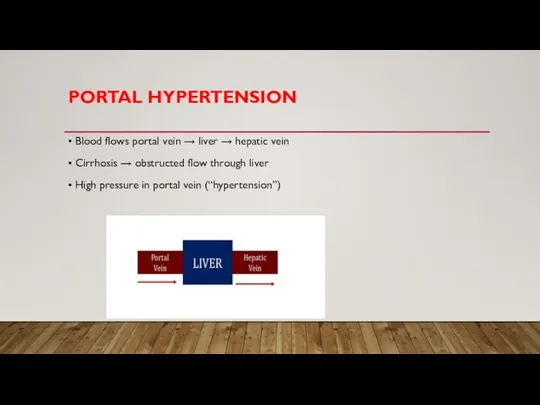
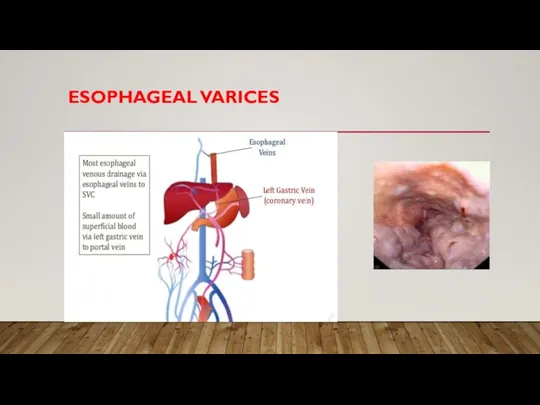
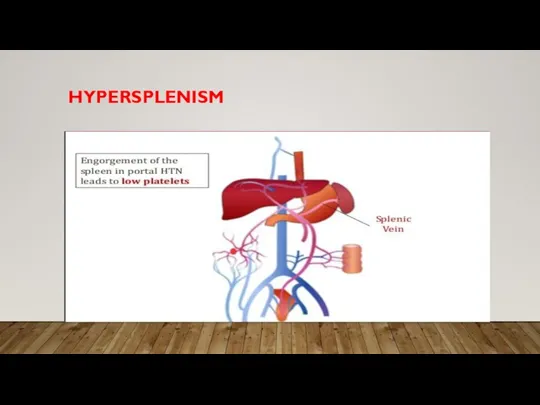
Слайд 9PORTAL HYPERTENSION
• Blood flows portal vein → liver → hepatic vein
• Cirrhosis
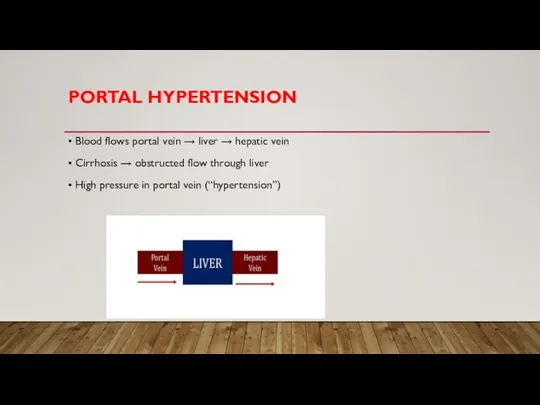
→ obstructed flow through liver
• High pressure in portal vein (“hypertension”)
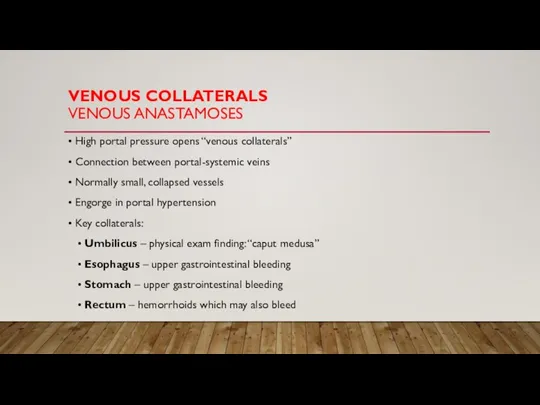
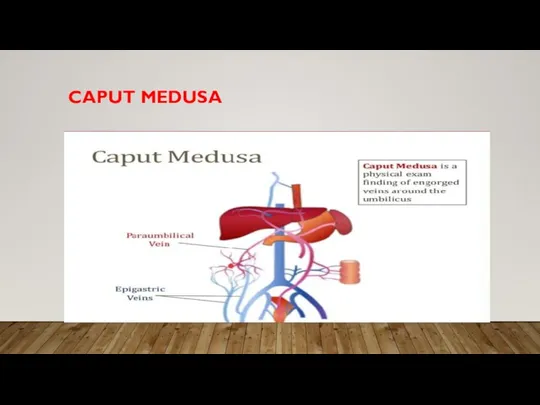
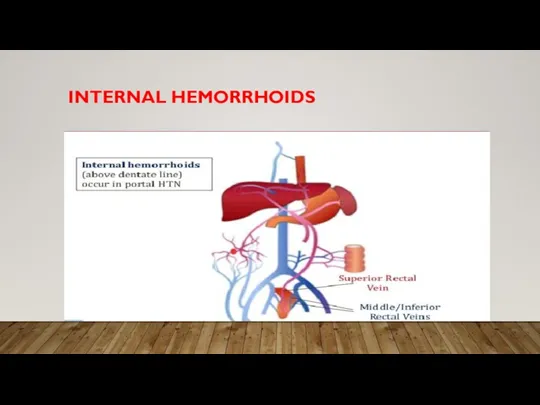
Слайд 12VENOUS COLLATERALS
VENOUS ANASTAMOSES
• High portal pressure opens “venous collaterals”
• Connection between
portal-systemic veins
• Normally small, collapsed vessels
• Engorge in portal hypertension
• Key collaterals:
• Umbilicus – physical exam finding: “caput medusa”
• Esophagus – upper gastrointestinal bleeding
• Stomach – upper gastrointestinal bleeding
• Rectum – hemorrhoids which may also bleed
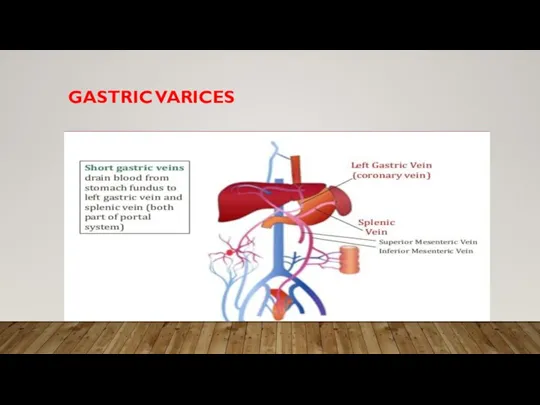
Слайд 18PORTAL VEIN THROMBOSIS
• Rare cause of portal hypertension
• Acute onset abdominal
pain
• Splenomegaly (palpable spleen one exam)
• May result in gastric varices with bleeding
• Liver biopsy will be normal
Слайд 19ASCITES
• Accumulation of fluid in peritoneal cavity
• In liver disease, from
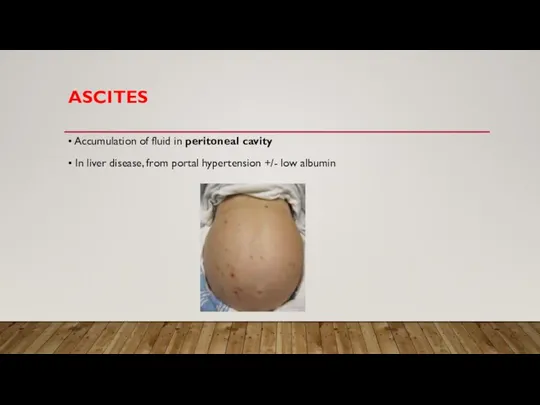
portal hypertension +/- low albumin
Слайд 20SAAG
SERUM ASCITES ALBUMIN GRADIENT
• Test of ascitic fluid
• Two reasons
for new/worsening ascites
• Portal hypertension
• Malignancy (leaky vasculature)
• Sample of ascitic fluid via paracentesis
• Serum albumin – ascites albumin = SAAG
Слайд 21SAAG
SERUM ASCITES ALBUMIN GRADIENT
• SAAG >1.1 g/dL
• Large difference
between serum and ascites albumin
• High pressure driving fluid (not albumin) into peritoneum
• Seen in portal hypertension
SAAG <1.1 g/Dl
Albumin levels similar between serum and ascites
• Leaky vasculature leading to fluid/albumin into peritoneum
Seen in malignant ascites (malignant cells in peritoneal cavity)
Слайд 22ASCITES TREATMENT
• Sodium restriction
• Spironolactone (drug of choice)
• Potassium-sparing diuretic
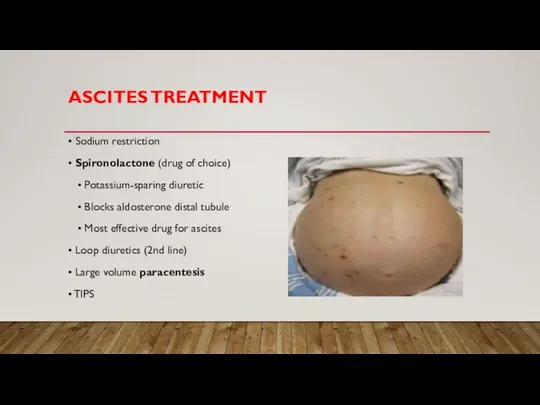
• Blocks aldosterone distal tubule
• Most effective drug for ascites
• Loop diuretics (2nd line)
• Large volume paracentesis
• TIPS
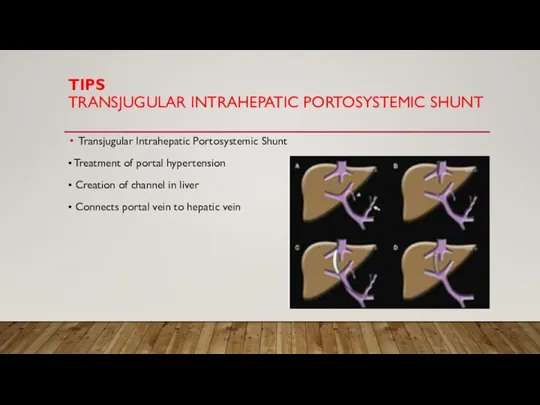
Слайд 23TIPS
TRANSJUGULAR INTRAHEPATIC PORTOSYSTEMIC SHUNT
Transjugular Intrahepatic Portosystemic Shunt
• Treatment of portal
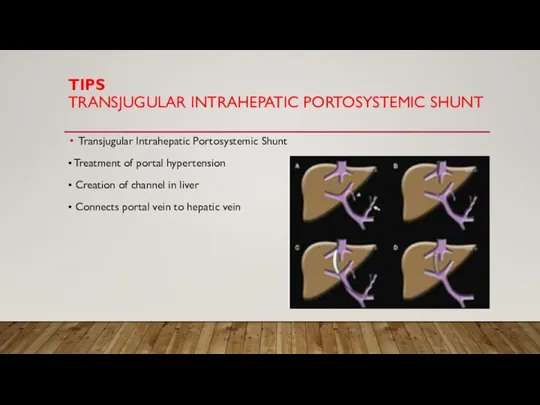
hypertension
• Creation of channel in liver
• Connects portal vein to hepatic vein
Слайд 24SBP
SPONTANEOUS BACTERIAL PERITONITIS
• Ascitic fluid infection
• Bacteria in gut gain
entry into ascitic fluid
• Usually E. coli and Klebsiella; rarely strep/staph
• Fever, abdominal pain/tenderness
• ↑ ascitic absolute PMNs (≥250 cells/mm3)
• Common treatment:
• 3rd generation cephalosporin (cefotaxime)
• Gram positive and gram negative coverage
• Achieves good levels in ascitic fluid
Слайд 25MELD SCORE
MODEL FOR END-STAGE LIVER DISEASE
• Scoring system for chronic liver
disease or cirrhosis
• Estimates 3-month mortality from liver disease
• Point system using:
• Bilirubin level
• Creatinine level
• INR
• >40 = 71% mortality
<9 = 2% mortality
Слайд 26CHILD-PUGH CLASSIFICATION
• Five variables to predict risk/survival
• Points for encephalopathy,
ascites, bilirubin, albumin, PT
• Score ranges from 5 to 15
• 5 or 6: Child-Pugh class A cirrhosis
• 7 to 9: Child-Pugh class B cirrhosis
• 10 to 15: Child-Pugh class C cirrhosis (worst)
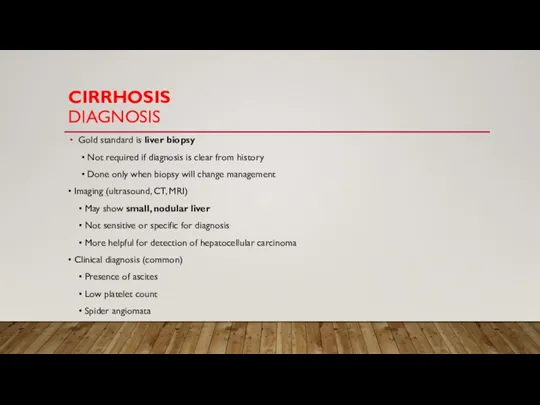
Слайд 27CIRRHOSIS
DIAGNOSIS
Gold standard is liver biopsy
• Not required if diagnosis is
clear from history
• Done only when biopsy will change management
• Imaging (ultrasound, CT, MRI)
• May show small, nodular liver
• Not sensitive or specific for diagnosis
• More helpful for detection of hepatocellular carcinoma
• Clinical diagnosis (common)
• Presence of ascites
• Low platelet count
• Spider angiomata
 Повреждение органов брюшной полости
Повреждение органов брюшной полости Патологияда тұқым қуалаушылықтың ролі
Патологияда тұқым қуалаушылықтың ролі Гипофиз
Гипофиз Роль плавания как одного из лучших средств для укрепления и закаливания организма
Роль плавания как одного из лучших средств для укрепления и закаливания организма Инфекционные заболевания
Инфекционные заболевания Иммунная система слизистых оболочек
Иммунная система слизистых оболочек Қазақ-ресей медицина университеті. Дерматовенерология кафедрасы
Қазақ-ресей медицина университеті. Дерматовенерология кафедрасы Mikrobiota_cheloveka
Mikrobiota_cheloveka tem-dien-tu-slide-gioi-thieu-san-pham-tem-xac-thuc-thong-minh-esafe
tem-dien-tu-slide-gioi-thieu-san-pham-tem-xac-thuc-thong-minh-esafe Тестовая программа. Правильные привычки питания
Тестовая программа. Правильные привычки питания Понятие здоровья. Биологический потенциал здоровья
Понятие здоровья. Биологический потенциал здоровья Топографическая анатомия таза и промежности
Топографическая анатомия таза и промежности Plastic surgery. Complications
Plastic surgery. Complications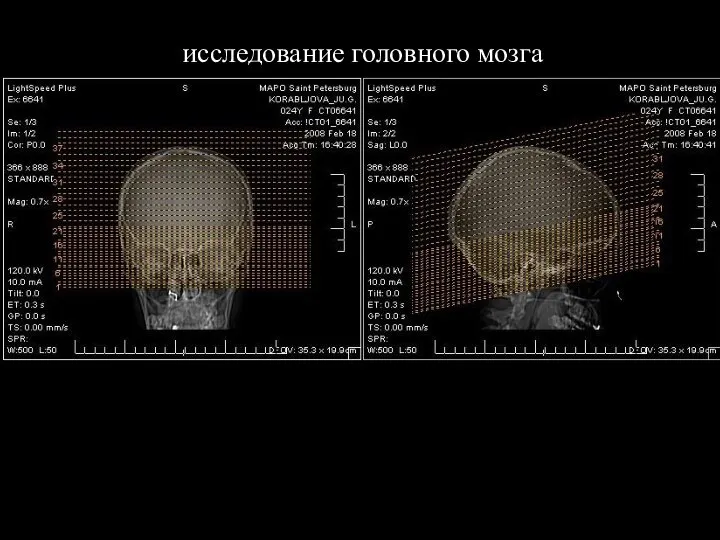 Магнитно-резонансная томография (МРТ), снимки
Магнитно-резонансная томография (МРТ), снимки Узнай свой биологический возраст
Узнай свой биологический возраст Организация психиатрической помощи в Российской Федерации. Сестринский процесс в психиатрии
Организация психиатрической помощи в Российской Федерации. Сестринский процесс в психиатрии Современные принципы диагностики и терапии легочной артериальной гипертензии
Современные принципы диагностики и терапии легочной артериальной гипертензии Виды медицинского страхования
Виды медицинского страхования Рецептура с основами технологии изготовления лекарственных форм
Рецептура с основами технологии изготовления лекарственных форм Су-джок терапия в коррекции речевых нарушений
Су-джок терапия в коррекции речевых нарушений Неотложные состояния в гинекологии
Неотложные состояния в гинекологии Надпеченочная желтуха
Надпеченочная желтуха Беременность и туберкулез
Беременность и туберкулез Другие ситуации, требующие оказания первой помощи
Другие ситуации, требующие оказания первой помощи Анатомия человека. Понятие о норме, аномалиях и пороках развития. Ткани, органы, системы органов
Анатомия человека. Понятие о норме, аномалиях и пороках развития. Ткани, органы, системы органов Пиелонефрит и цистит у детей
Пиелонефрит и цистит у детей Сокращения: КФ – клиническая фармакология, ЛС – лекарственное средство, ЛП – лекарственный препарат
Сокращения: КФ – клиническая фармакология, ЛС – лекарственное средство, ЛП – лекарственный препарат Травматизм, его основные виды
Травматизм, его основные виды