Содержание
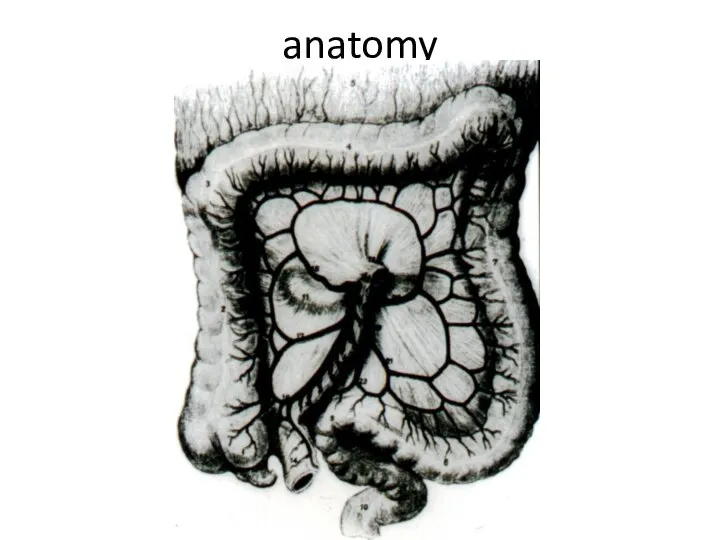
- 2. anatomy
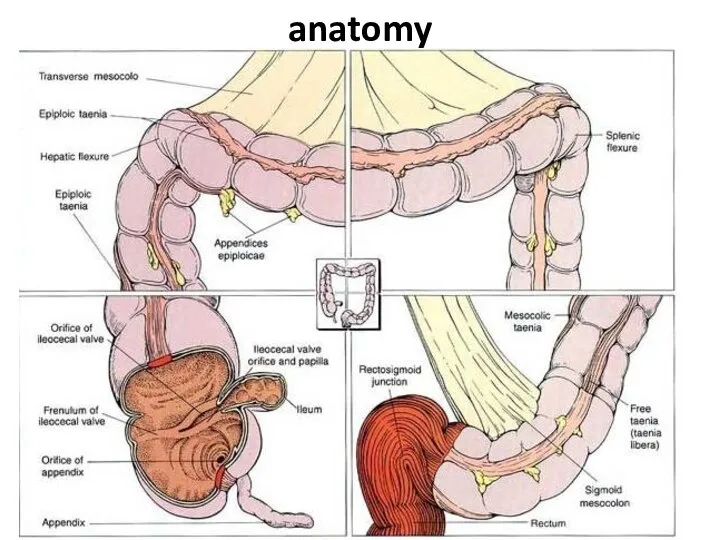
- 3. anatomy
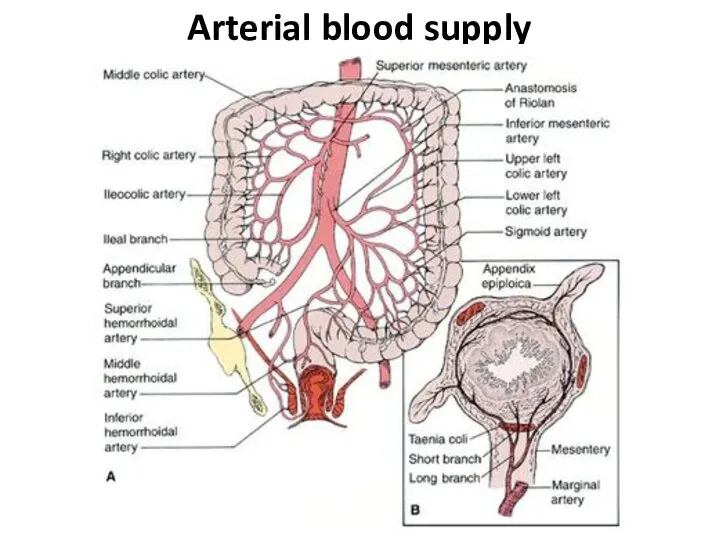
- 4. Arterial blood supply
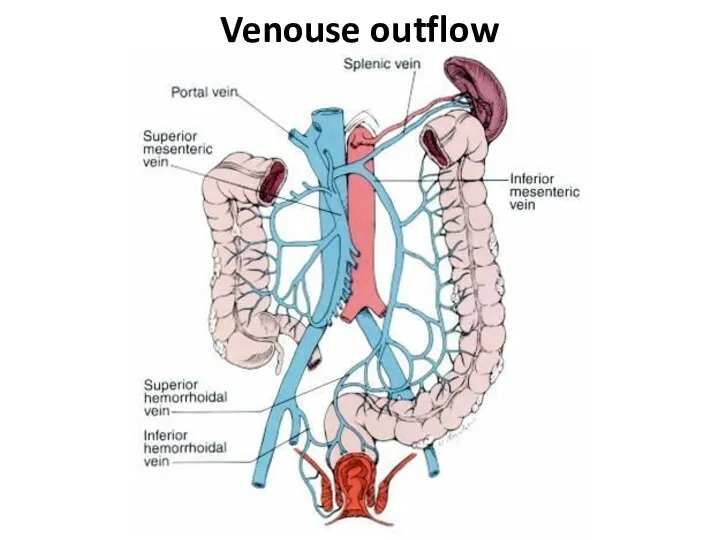
- 5. Venouse outflow
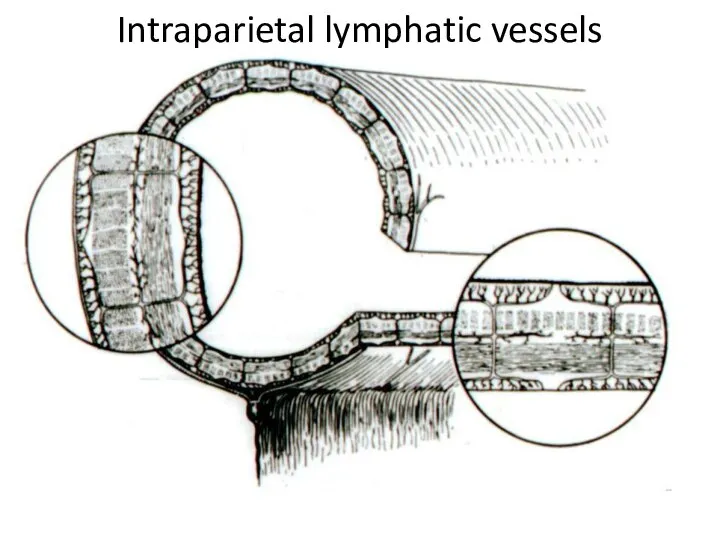
- 6. Intraparietal lymphatic vessels
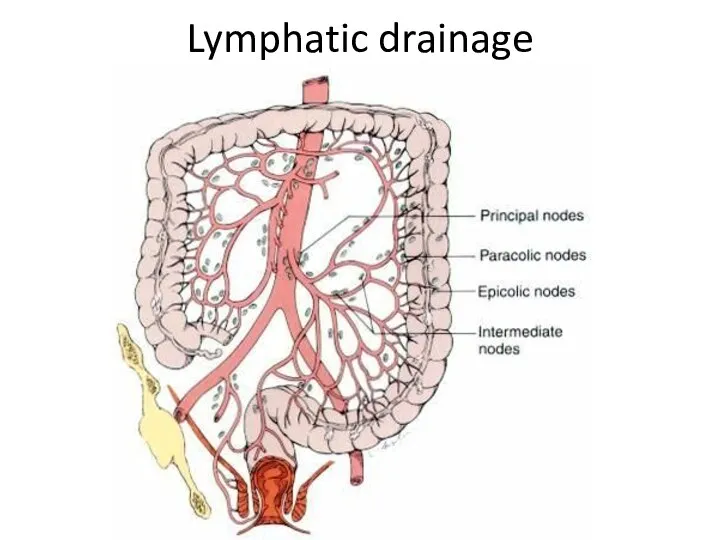
- 7. Lymphatic drainage
- 8. Differences of the right and left half Anatomy: on the right the lumen is wider, than
- 9. Special investigation methods 1. Physical investiga-tion 2. A proctosigmoido-scopy 3. Fibrocolonoscopy
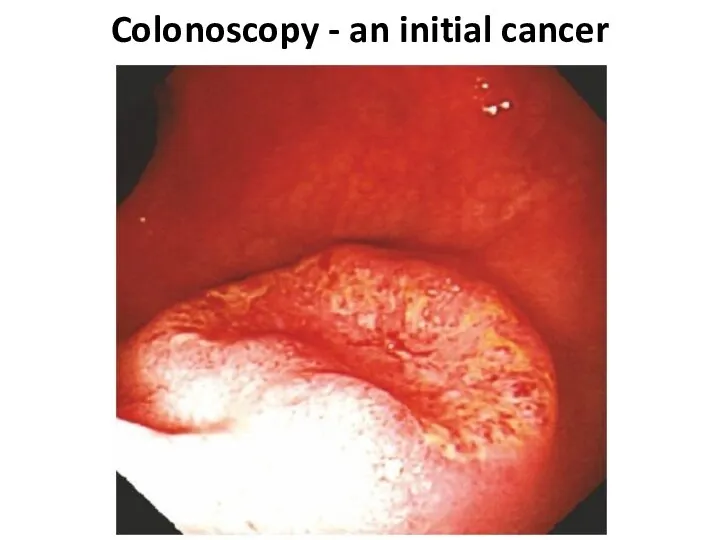
- 10. Colonoscopy - an initial cancer
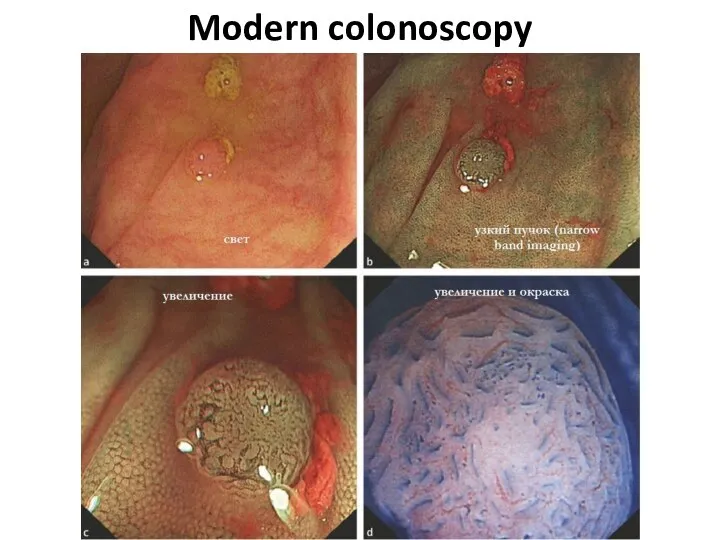
- 11. Modern colonoscopy
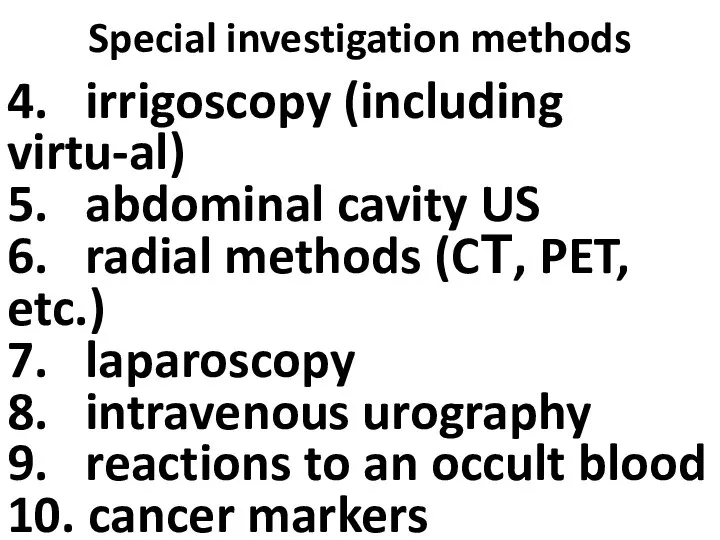
- 12. Special investigation methods 4. irrigoscopy (including virtu-al) 5. abdominal cavity US 6. radial methods (CТ, PET,
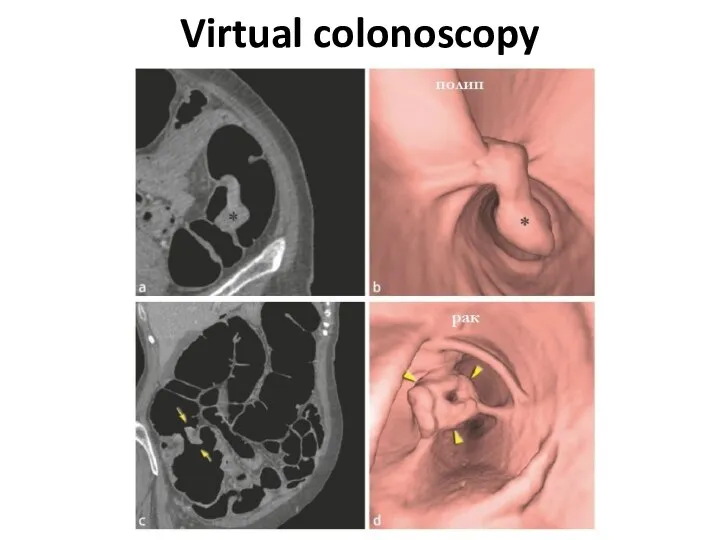
- 13. Virtual colonoscopy
- 14. At what a cancer localization more often anemy?
- 15. At what a cancer localization more often Visible bleeding?
- 16. AT WHAT A CANCER LOCALIZATION MORE OFTEN Disturbance of passability
- 17. AT WHAT A CANCER LOCALIZATION MORE OFTEN Perforation is more possible?
- 18. AT WHAT A CANCER LOCALIZATION MORE OFTEN Fistulas, phlegmons are possible?
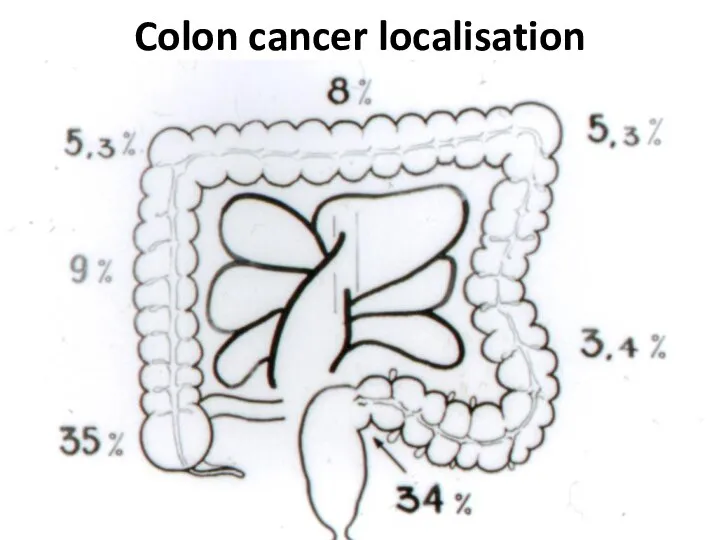
- 19. Colon cancer localisation
- 20. Cancer clinical signs 1. Functional signs without intestinal disorders (a pain, etc.) 2. Intestinal disorders (diarrheas,
- 21. Cancer clinical forms 1) toxico-anemic 2) enterocolitic 3) dyspeptic 4) obturational 5) pseudo-inflammatory 6) tumoral
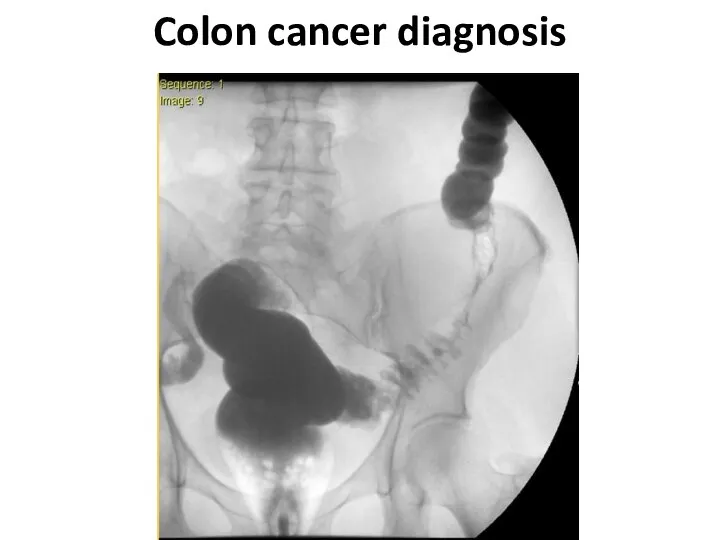
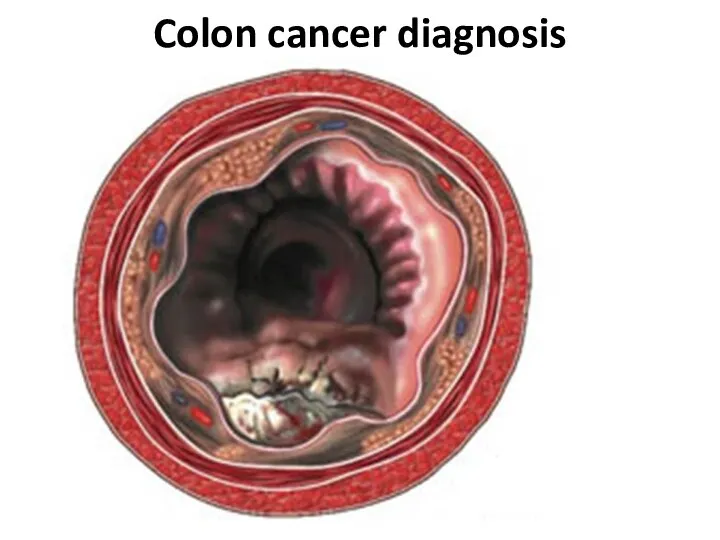
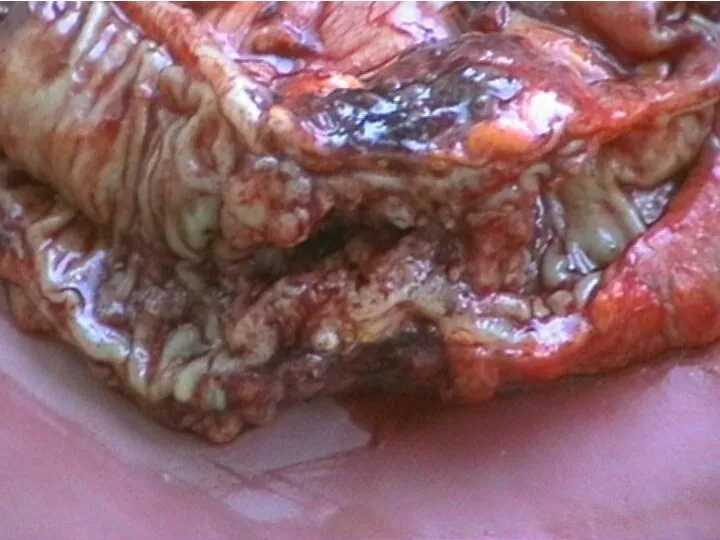
- 22. Colon cancer diagnosis
- 23. Colon cancer diagnosis
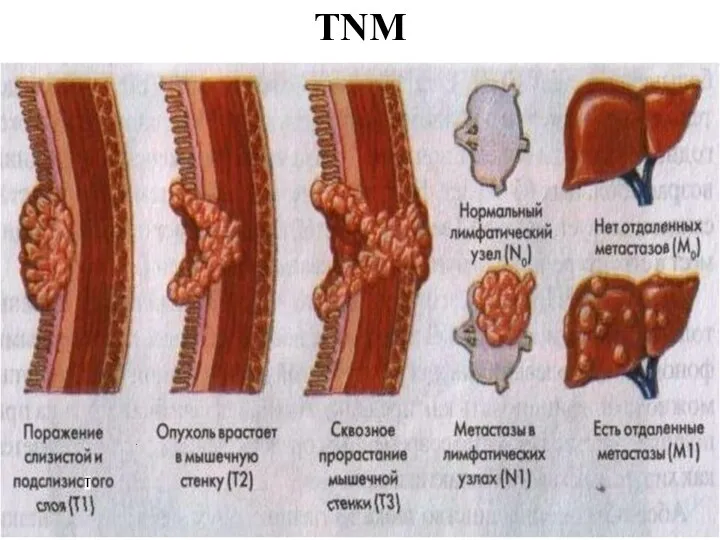
- 26. TNM
- 27. TNM - T Tx - the estimation of a primary tumour is impossible T0 - the
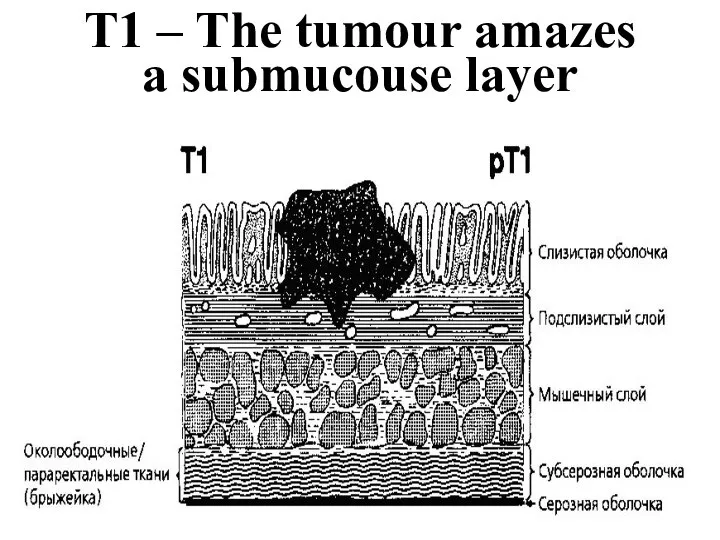
- 28. T1 – The tumour amazes a submucouse layer
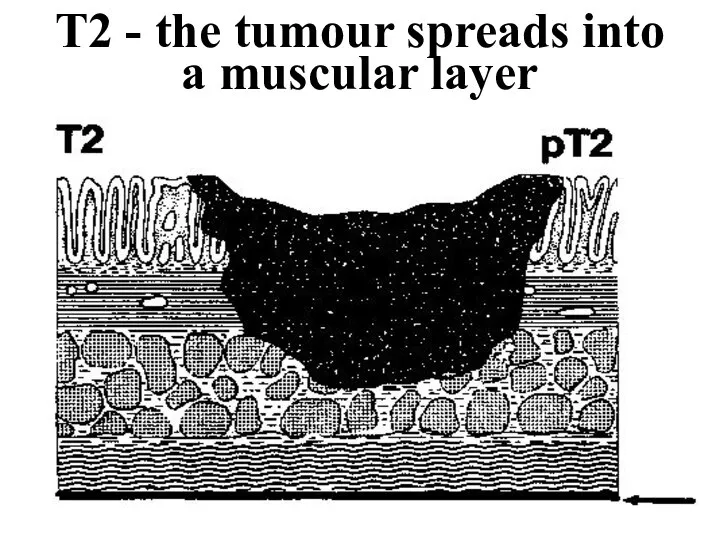
- 29. T2 - the tumour spreads into a muscular layer
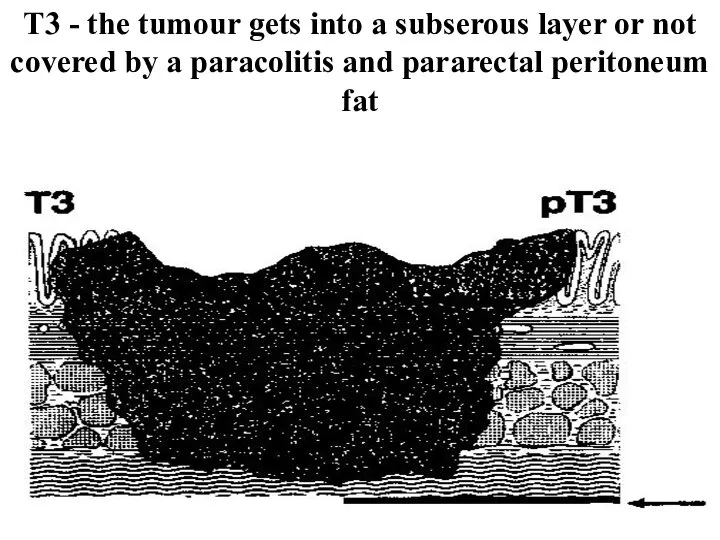
- 30. Т3 - the tumour gets into a subserous layer or not covered by a paracolitis and
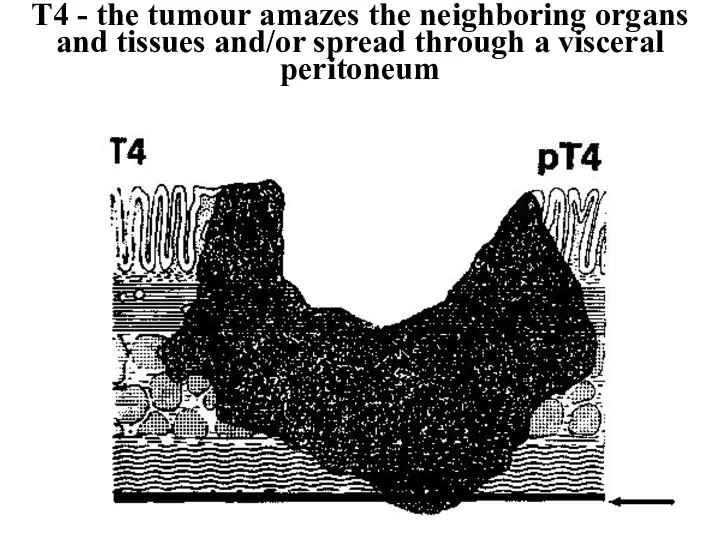
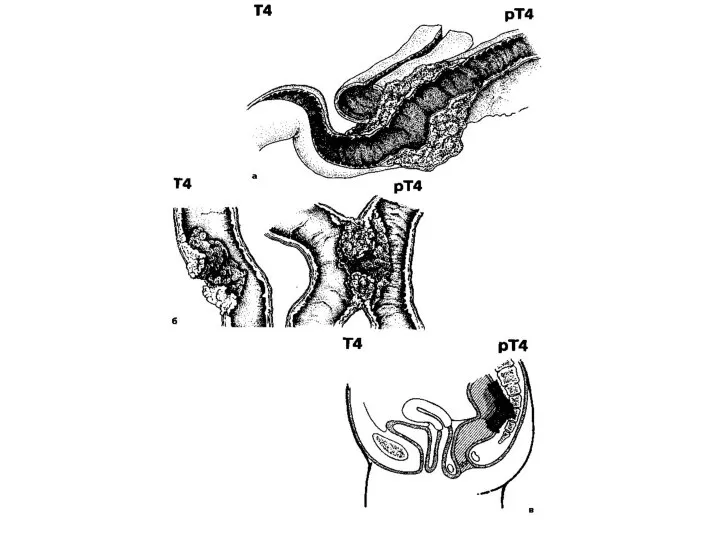
- 31. Т4 - the tumour amazes the neighboring organs and tissues and/or spread through a visceral peritoneum
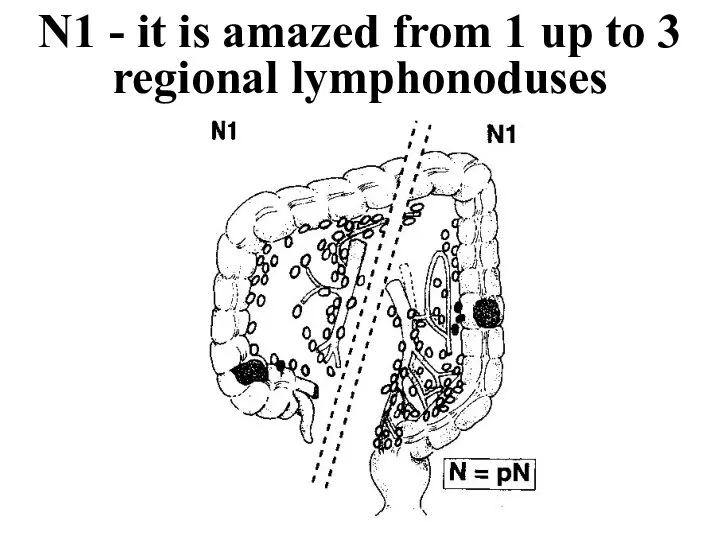
- 33. N1 - it is amazed from 1 up to 3 regional lymphonoduses
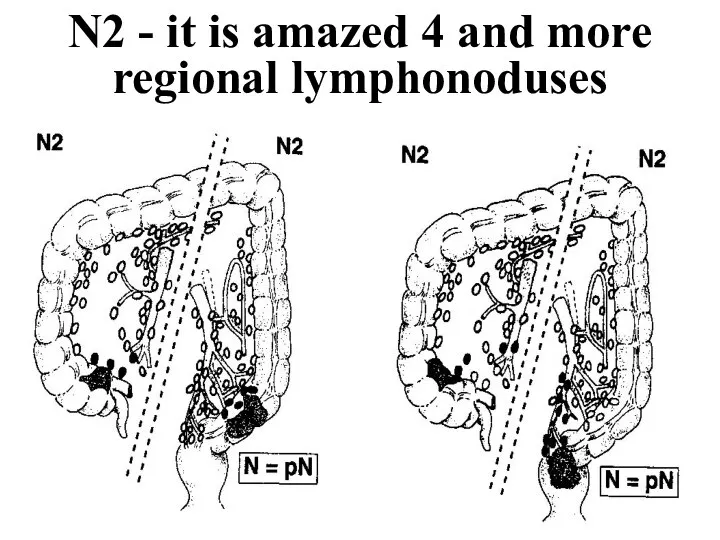
- 34. N2 - it is amazed 4 and more regional lymphonoduses
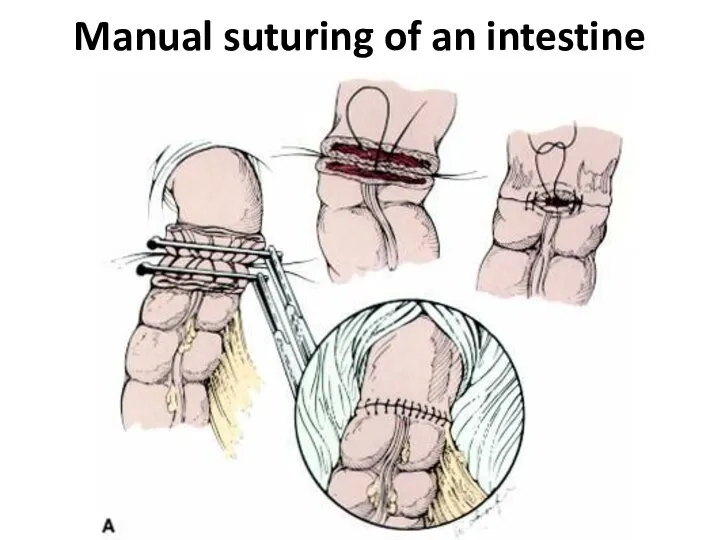
- 35. Manual suturing of an intestine
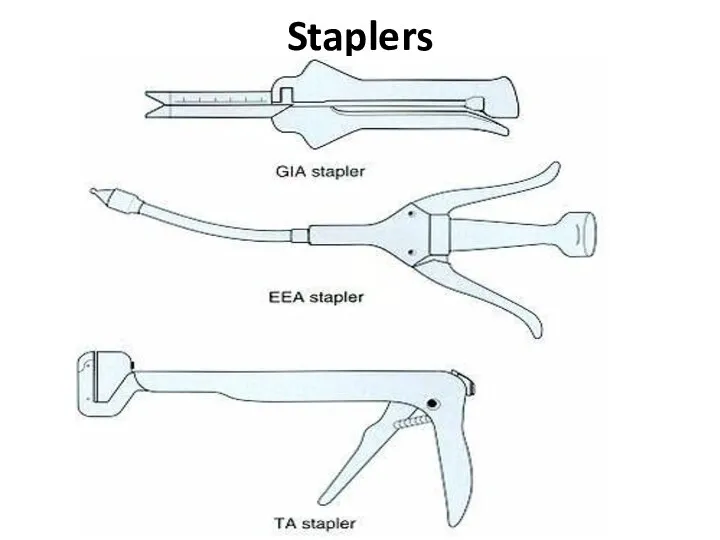
- 36. Staplers
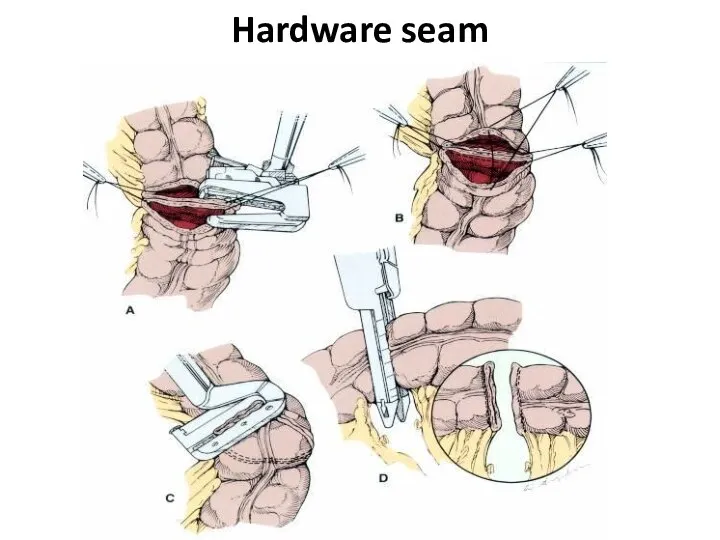
- 37. Hardware seam
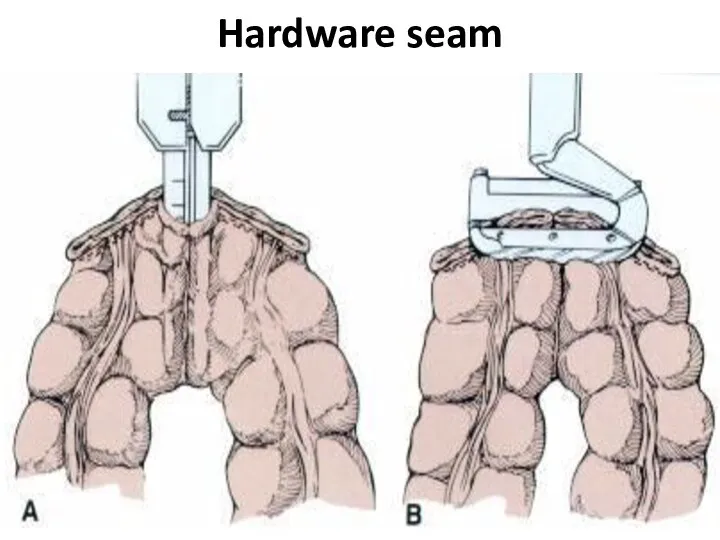
- 38. Hardware seam
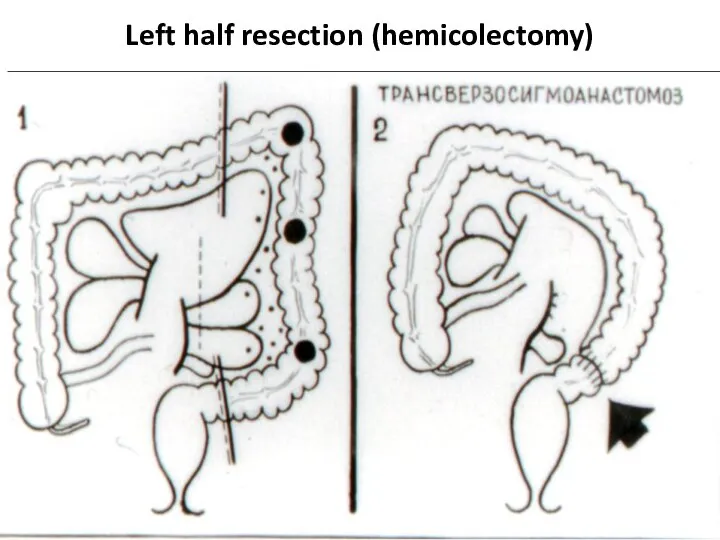
- 39. Left half resection (hemicolectomy)
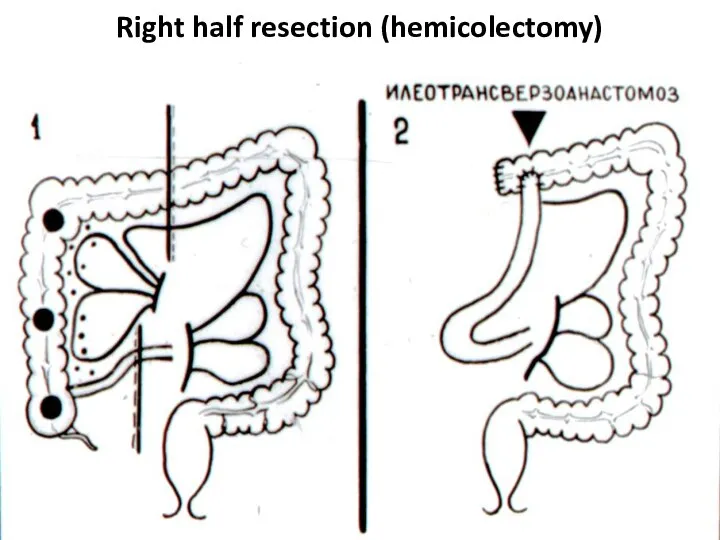
- 40. Right half resection (hemicolectomy)
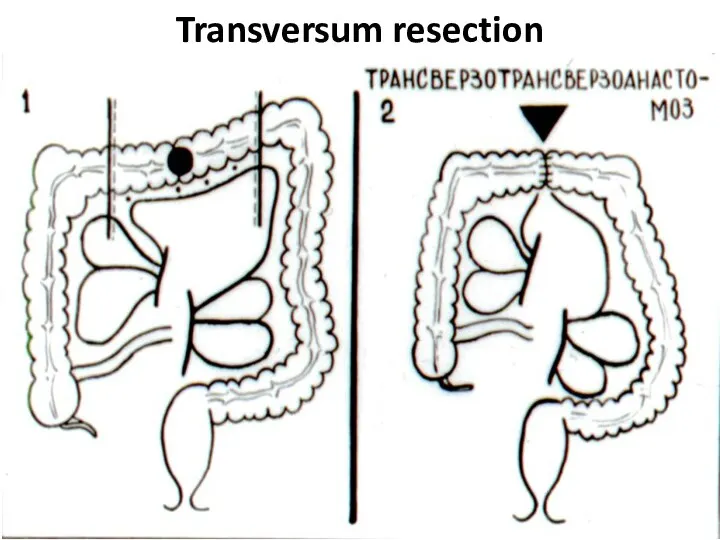
- 41. Transversum resection
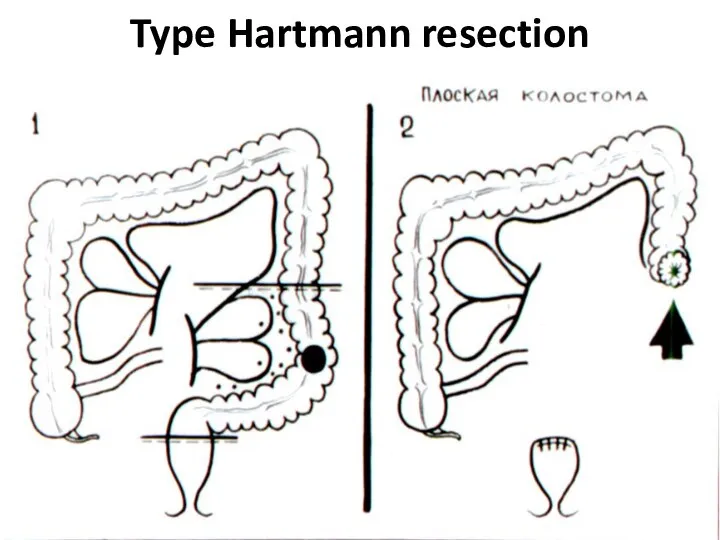
- 42. Type Hartmann resection
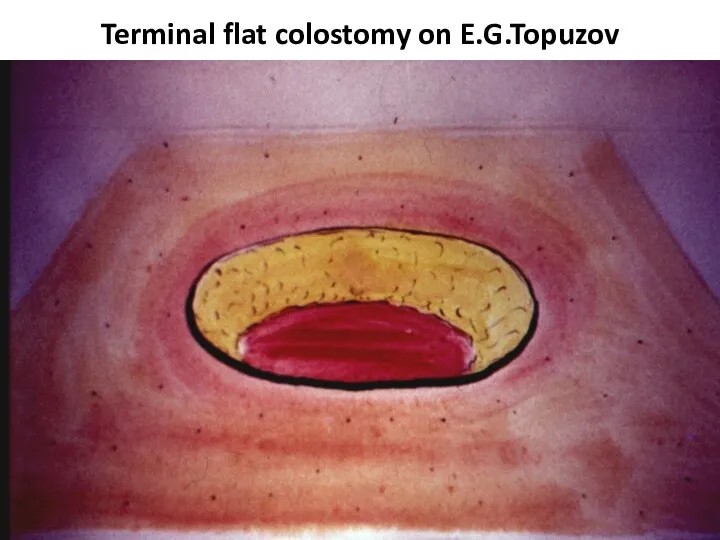
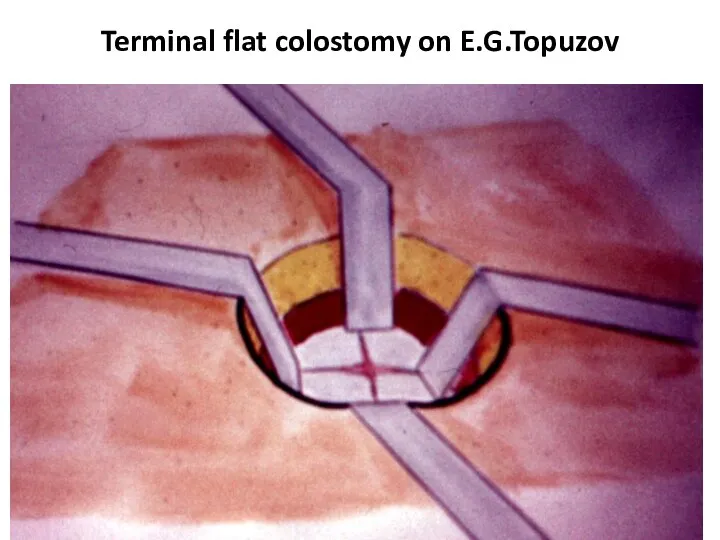
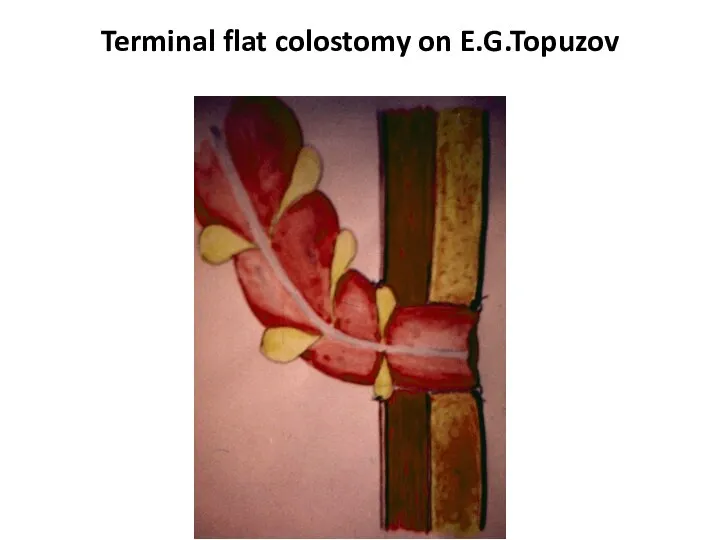
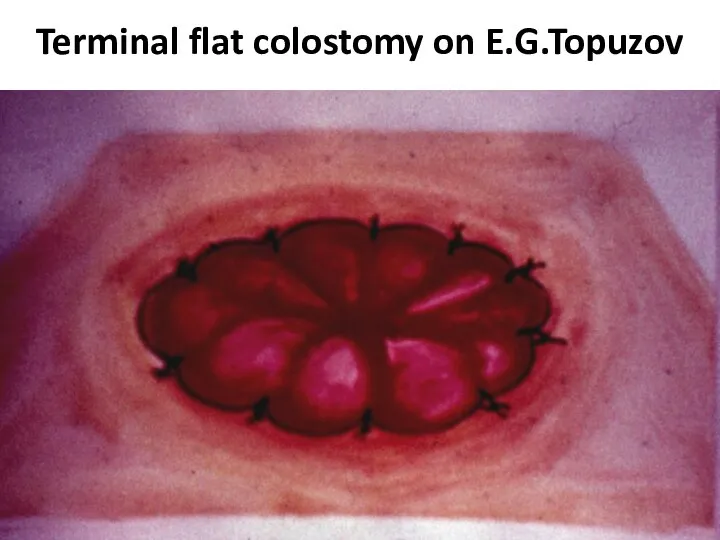
- 43. Terminal flat colostomy on E.G.Topuzov
- 44. Terminal flat colostomy on E.G.Topuzov
- 45. Terminal flat colostomy on E.G.Topuzov
- 46. Terminal flat colostomy on E.G.Topuzov
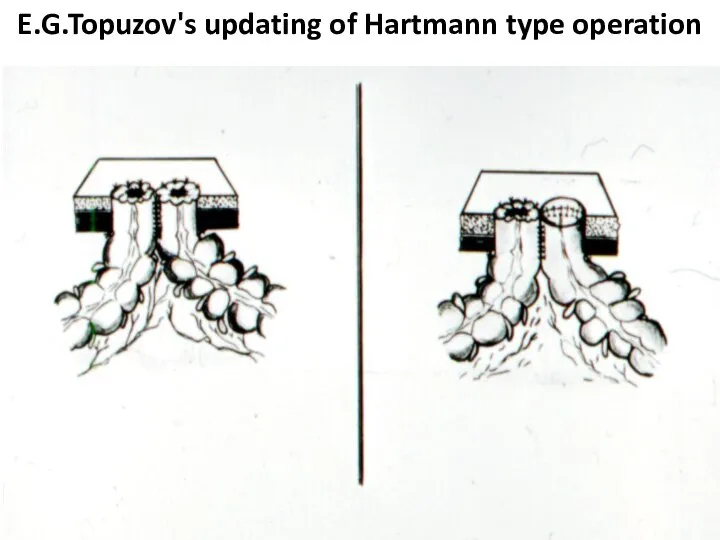
- 47. E.G.Topuzov's updating of Hartmann type operation
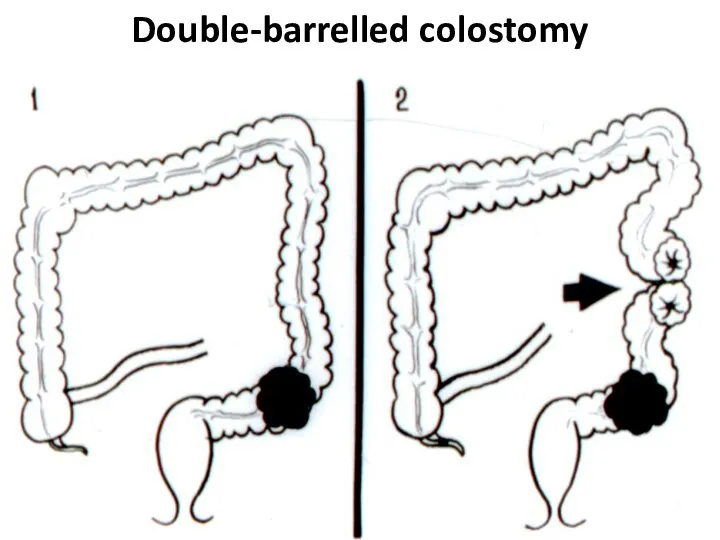
- 48. Double-barrelled colostomy
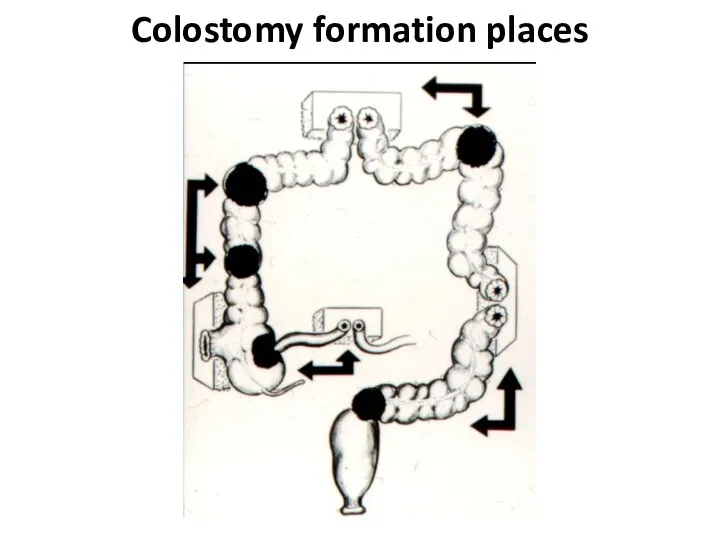
- 49. Colostomy formation places
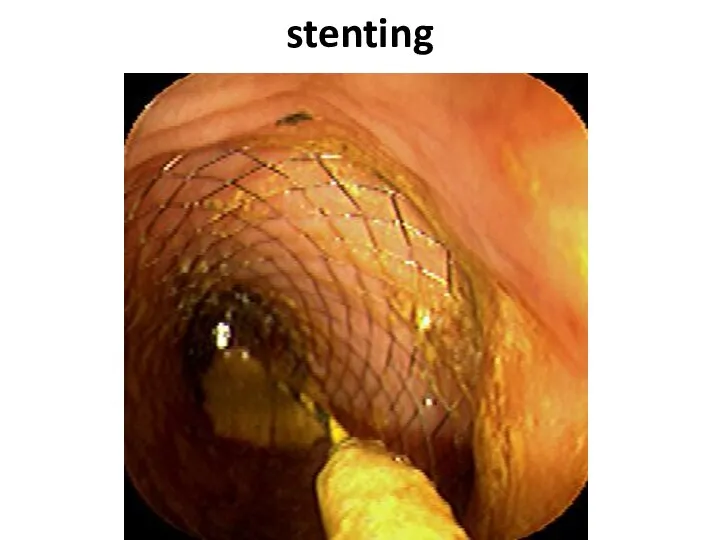
- 50. stenting
- 51. stenting
- 52. complications The intestinal obstruction is most typical for a tu-mor localization in the colon left half
- 53. complications The inflammation in tissues surrounding a tumour (up to phlegmon or abscess de-velopment) is marked
- 54. Question Pain in the right ileal region, a tumour and a heat. With what diseases you
- 55. complications Perforation of an intestine can be as in a zone of the tumour, at its
- 56. Question At what colon can-cer complication Schetkin-Blumberg sign more often is defined?
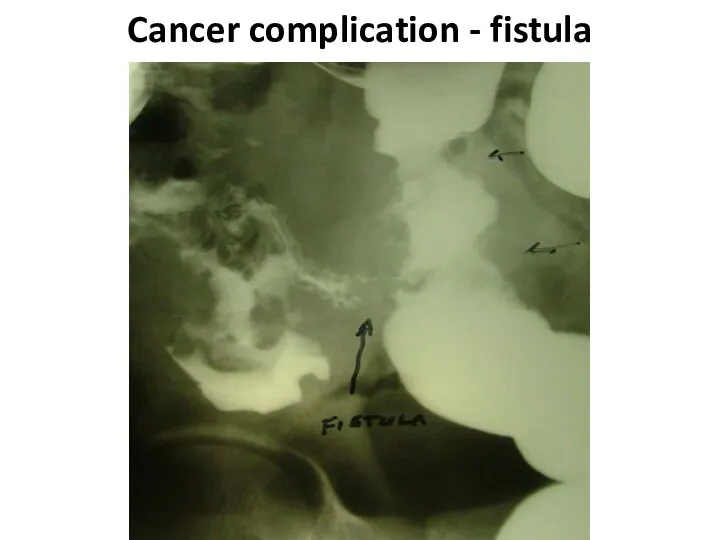
- 57. complications Formation of fistulas at spreading at the nea-rest hollow organs (co-lo-small intestinal, co-lo-gastric, colo-vesical) carry
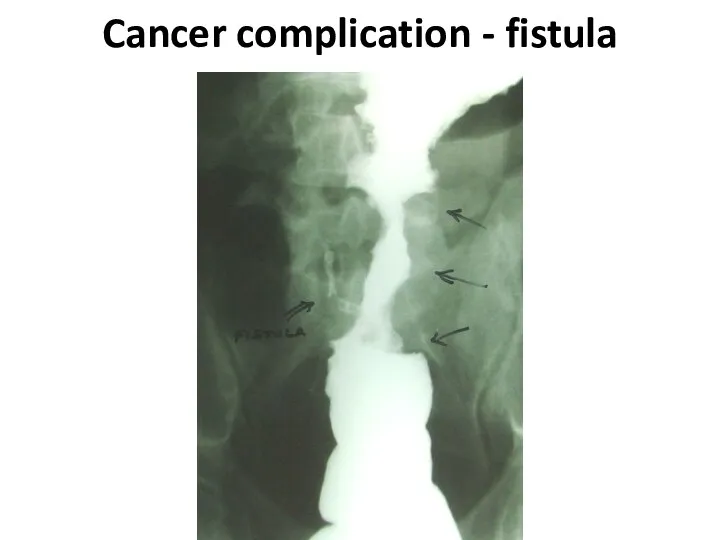
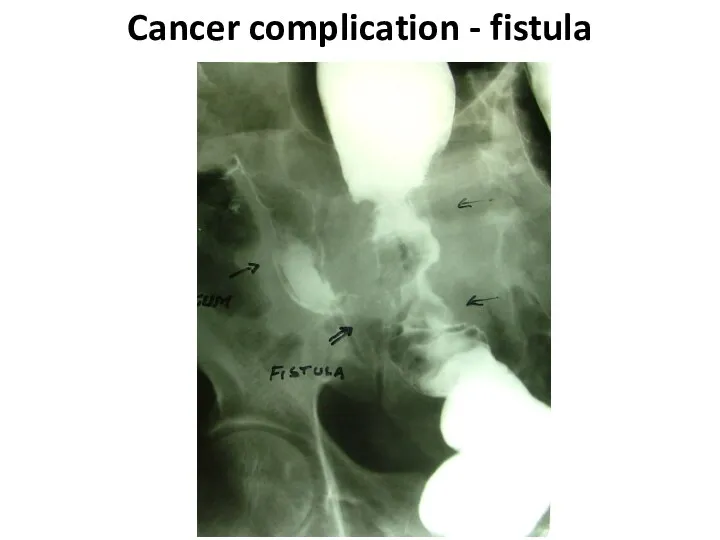
- 58. Cancer complication - fistula
- 59. Cancer complication - fistula
- 60. Cancer complication - fistula
- 61. complications The intestinal bleeding happens, as a rule, insig-nificant. Sometimes it is shown in the form
- 62. Colon diseases
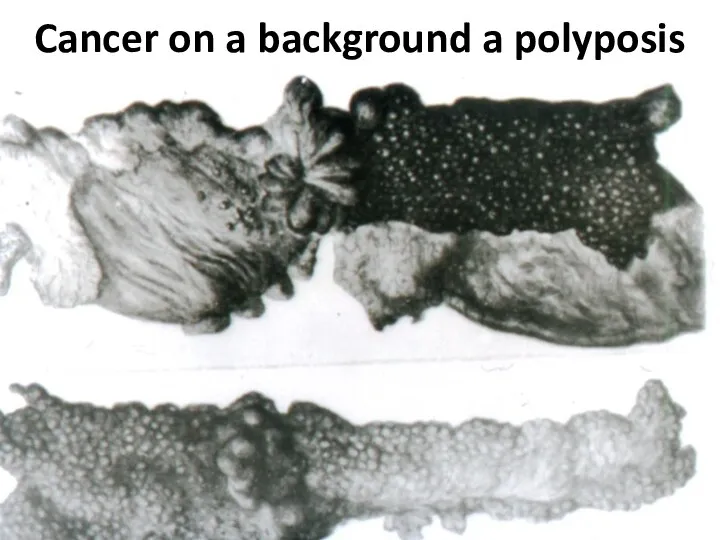
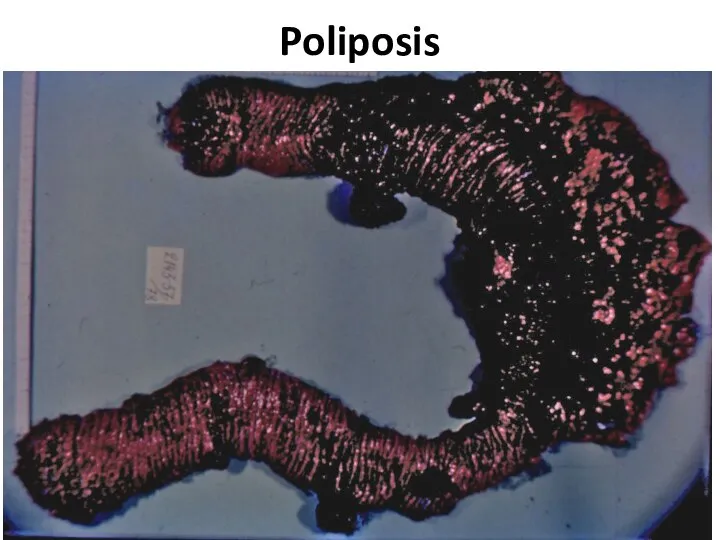
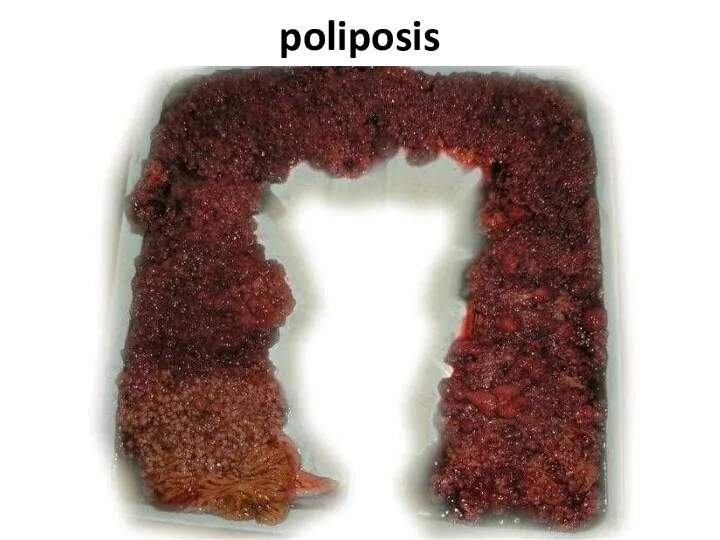
- 63. Cancer on a background a polyposis
- 64. Poliposis
- 65. Nonspecific colitises 1. Ulcerouse 2. Granulomatous (Crohn's disease) 3. Ischemic
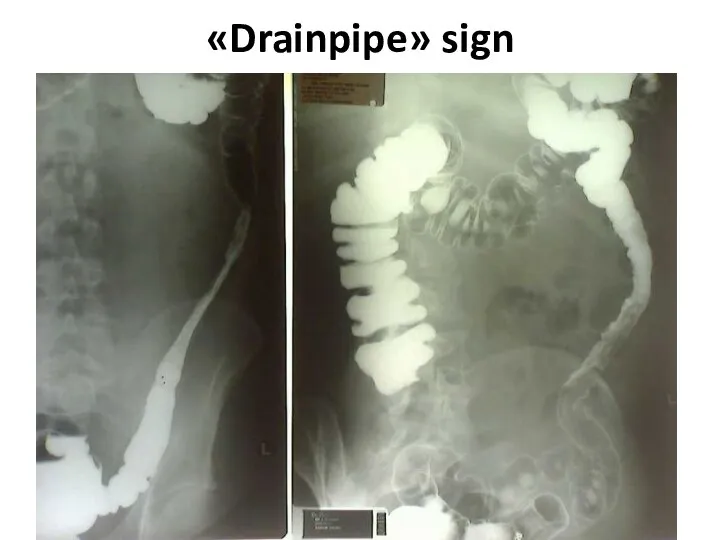
- 66. «Drainpipe» sign
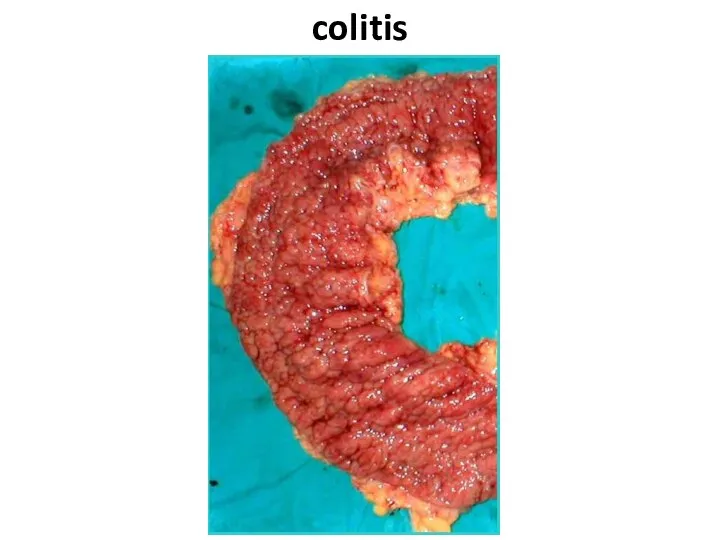
- 67. colitis
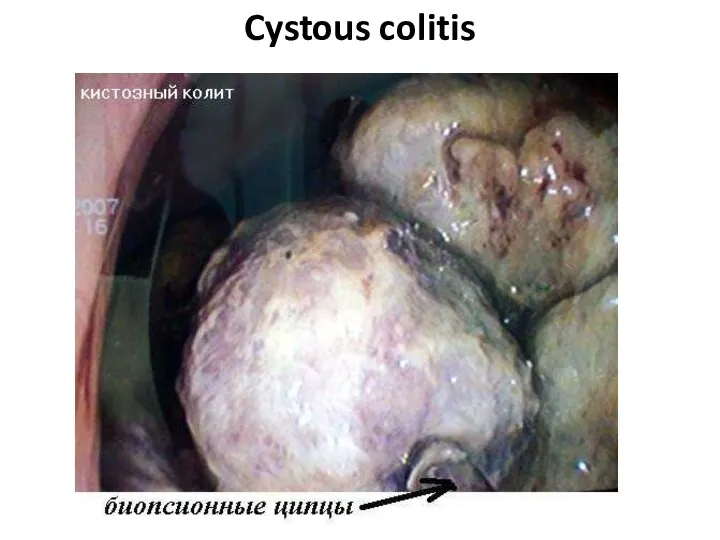
- 68. Cystous colitis
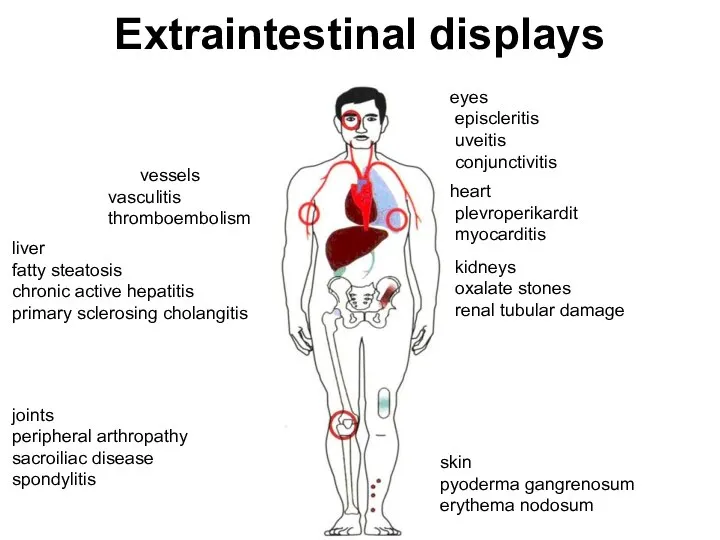
- 69. Extraintestinal displays vessels vasculitis thromboembolism liver fatty steatosis chronic active hepatitis primary sclerosing cholangitis joints peripheral
- 70. complications Toxic megacolon Perforation Peritonitis Intestinal obstruction Bleedings Abscesses Fistulas Infiltrates
- 71. Indications to operation at ulcerouse colitis Intestinal bleeding. 1. The frequency of bowel movements 12 or
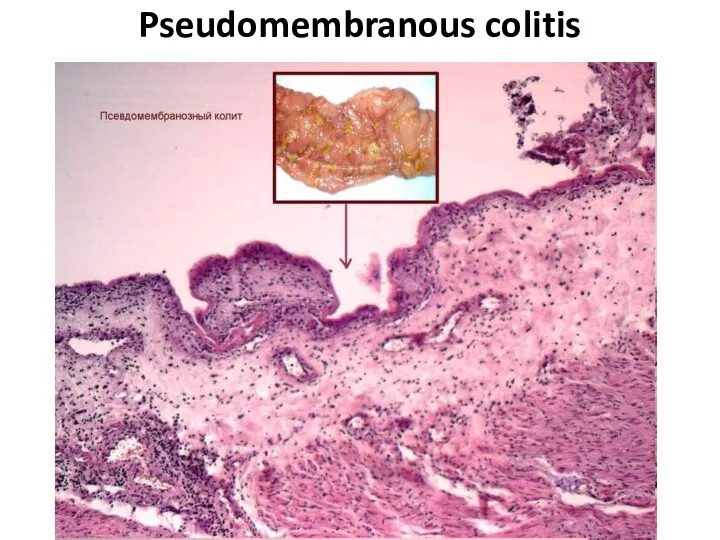
- 72. Pseudomembranous colitis
- 73. Polips Hyperplastic Tubular adenoma Tubulary-villiferous adenoma Villiferous adenoma
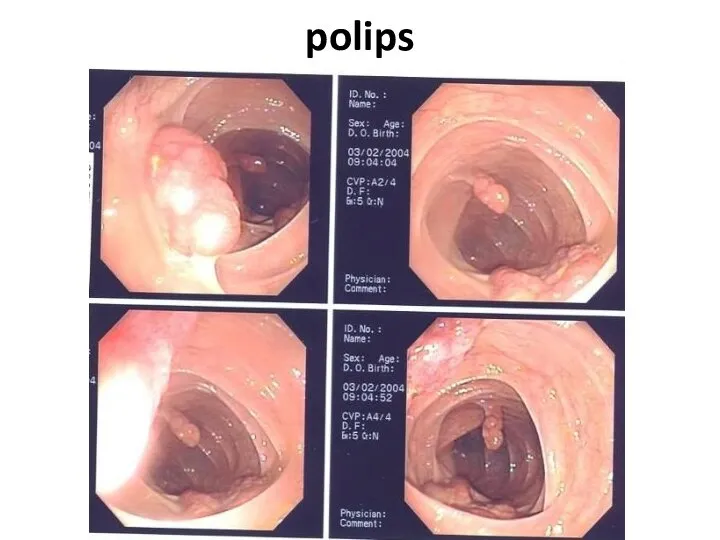
- 74. polips
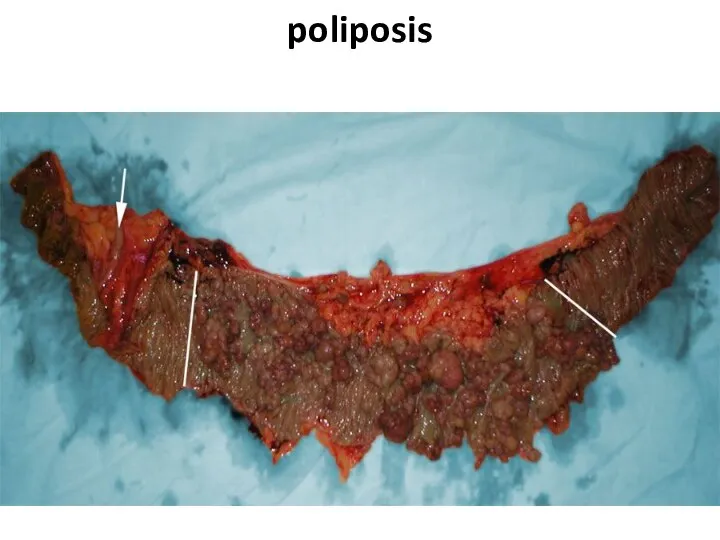
- 75. poliposis
- 76. poliposis
- 77. Congenital diseases 1. Hirshsprung disease 2. Megacolon 3. Dolichocolon
- 78. Hirshsprung disease
- 79. Differential diagnostics 1. Myxedema 2. Medicinal influences (morphinum and so forth) 5. Depressions 6. Schizophrenia 7.
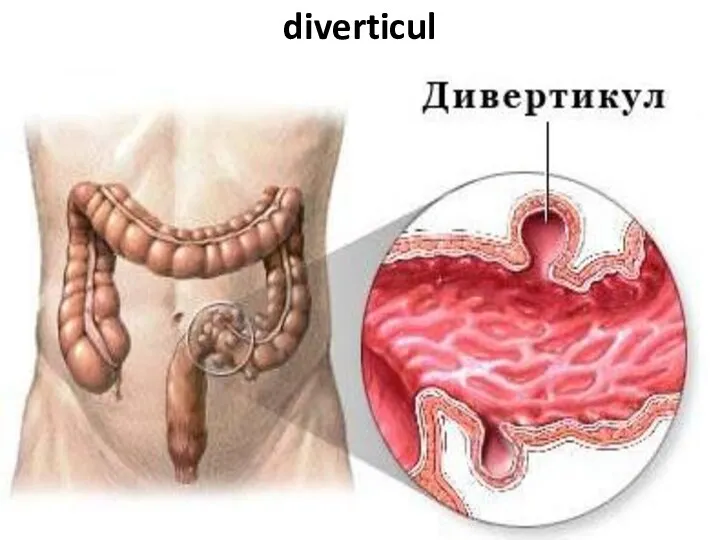
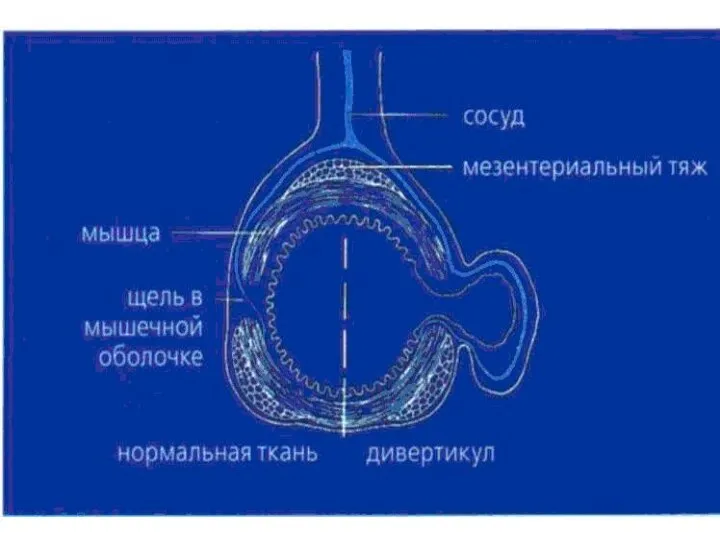
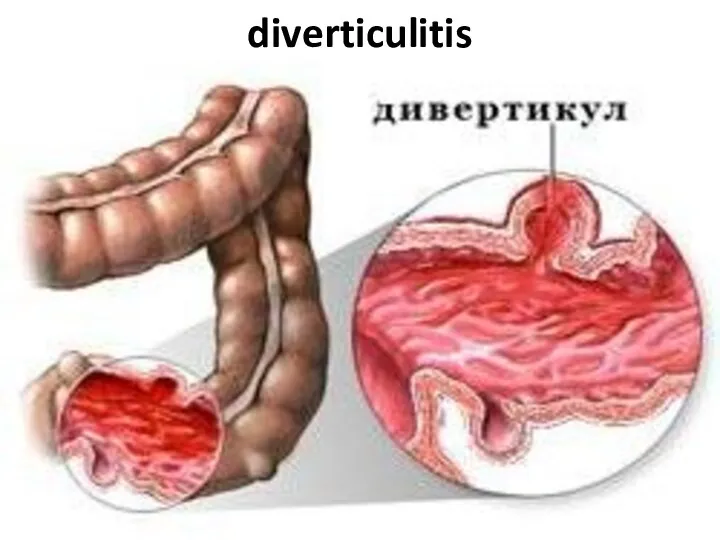
- 80. diverticuls Diverticul Diverticulosis Diverticulitis
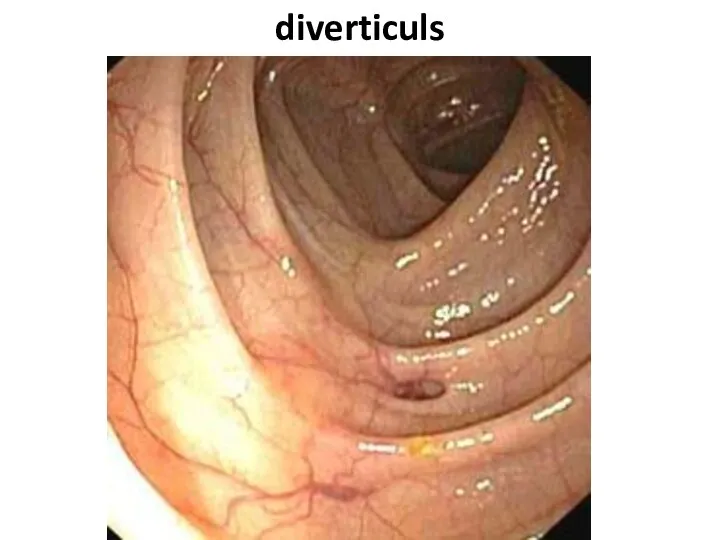
- 81. diverticul
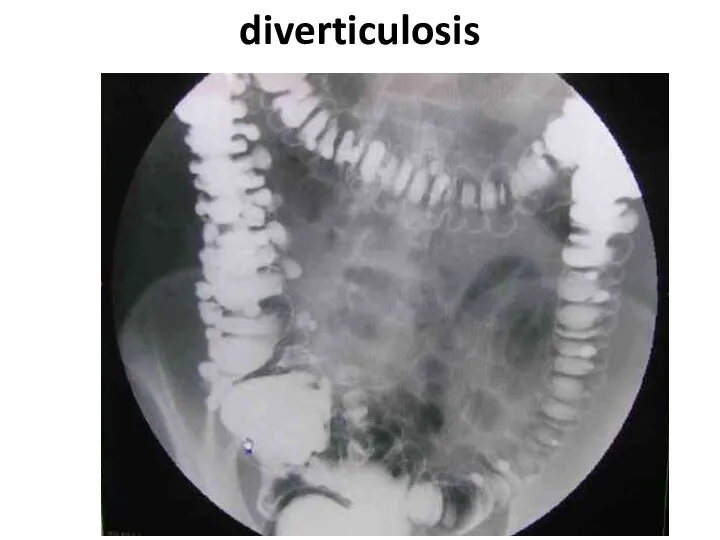
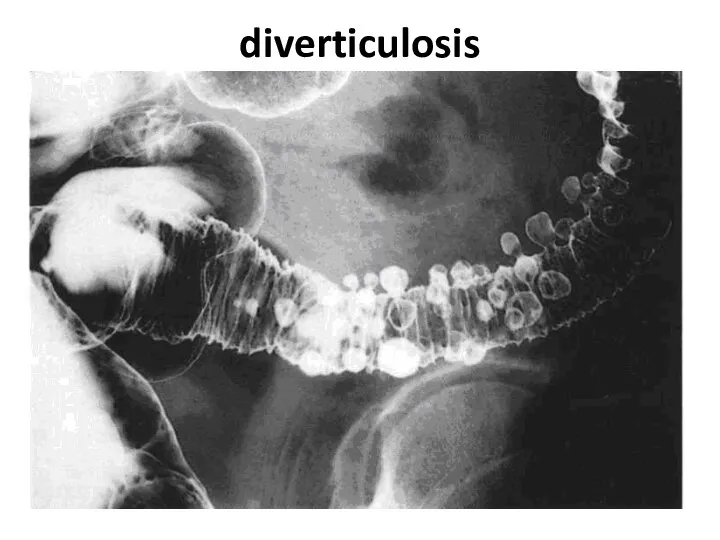
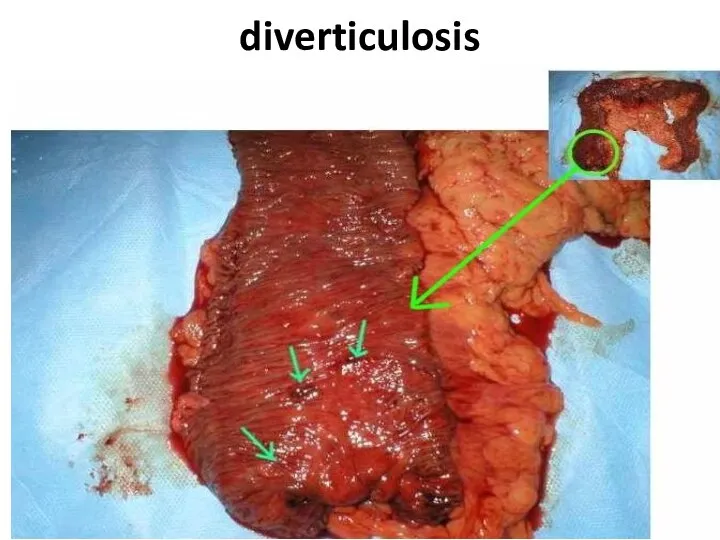
- 83. diverticulosis
- 84. diverticulosis
- 85. diverticuls
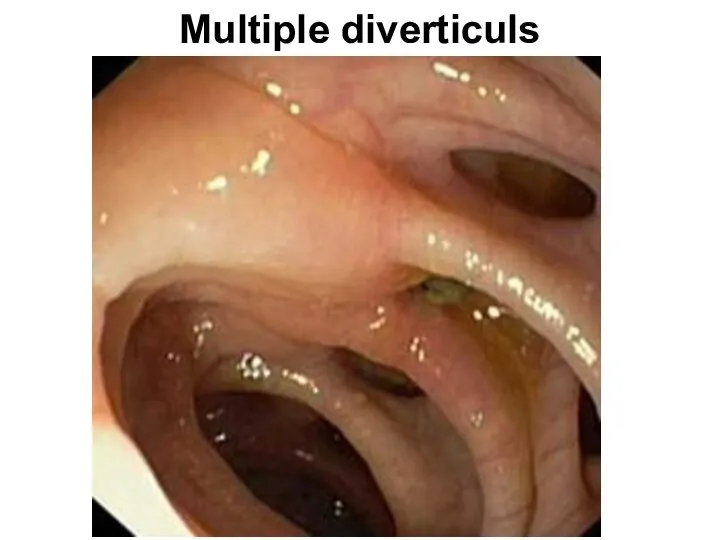
- 86. Multiple diverticuls
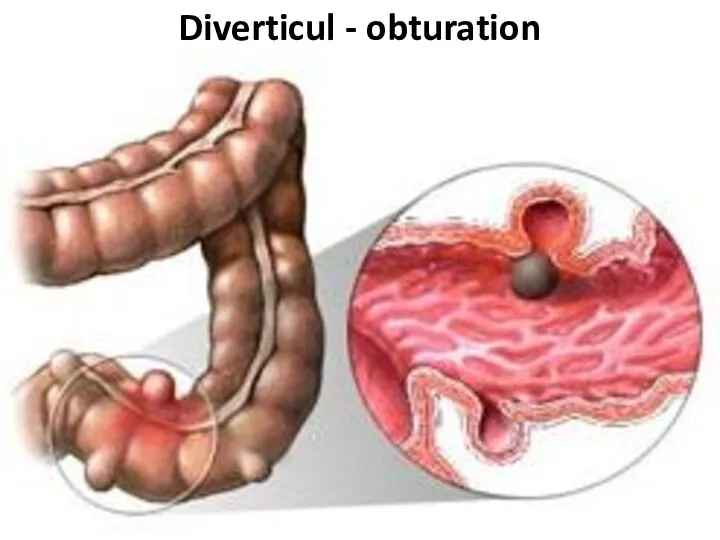
- 87. Diverticul - obturation
- 88. diverticulosis
- 89. Fecal stone in a diverticulum
- 90. diverticulitis
- 91. Clinical features Acute diverticulitis is well nicknamed 'left-sided appendicitis'; an acute onset of central abdominal pain
- 92. Clinical features Chronic divertlcular disease exactly mimics the local clinical features of carcinoma of the colon;
- 93. Diverticulitis This results from infection of one or more divertlcula. An inflamed diverticulum may. 1. Perforate:
- 94. Diverticulitis The Hinchey classification - proposed by Hinchey et al. in 1978[1] classifies a colonic perforation
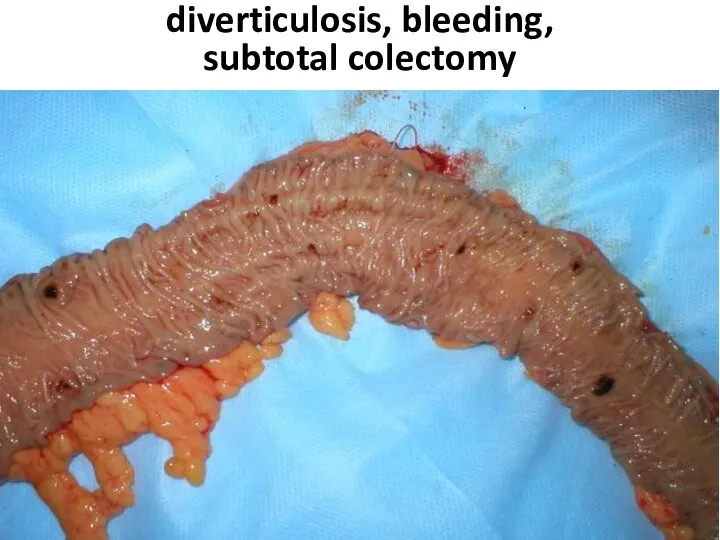
- 95. diverticulosis, bleeding, subtotal colectomy
- 96. diverticulosis, bleeding, subtotal colectomy
- 98. Скачать презентацию




![Diverticulitis The Hinchey classification - proposed by Hinchey et al. in 1978[1]](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/1165791/slide-93.jpg)

 Лекарственная непереносимость
Лекарственная непереносимость Микробиологическая диагностика энтеробактерий
Микробиологическая диагностика энтеробактерий Индралин (Б-190)
Индралин (Б-190) Кишечная непроходимость
Кишечная непроходимость Балалардағы пародонт аурулары
Балалардағы пародонт аурулары Рак мочевого пузыря и его лечение
Рак мочевого пузыря и его лечение Вступление к TCCC. Тактическая помощь пострадавшим в бою для медицинского персонала
Вступление к TCCC. Тактическая помощь пострадавшим в бою для медицинского персонала Хронической лимфоцитарный лейкоз
Хронической лимфоцитарный лейкоз Эпидмониторинг
Эпидмониторинг Хроническая воспалительная демиелинизирующая полинейропатия
Хроническая воспалительная демиелинизирующая полинейропатия Аллергия. Аллергические реакции
Аллергия. Аллергические реакции Дезинфекция и стерилизация изделий медицинского назначения
Дезинфекция и стерилизация изделий медицинского назначения Медицинская помощь и ее виды. Военная медицина
Медицинская помощь и ее виды. Военная медицина Клебсиеллалар, микоплазмалар. Сипаттамасы. Қасиеттері. Диагноз қою, алдын алу, емдеу
Клебсиеллалар, микоплазмалар. Сипаттамасы. Қасиеттері. Диагноз қою, алдын алу, емдеу Левин
Левин Несовершенный амелогенез и дентиногенез
Несовершенный амелогенез и дентиногенез 230921_201532_palypaciya-perkussii-auskulytaciya
230921_201532_palypaciya-perkussii-auskulytaciya Фитоэстрин. Негормональный комплекс для женщин
Фитоэстрин. Негормональный комплекс для женщин Холера. Клиника, диагностика, лечение
Холера. Клиника, диагностика, лечение Качественная диспансеризация как инструмент улучшения демографических показателей
Качественная диспансеризация как инструмент улучшения демографических показателей Патология обмена веществ в органах и тканях
Патология обмена веществ в органах и тканях Эвакуационных мероприятий больных или лиц с подозрением на COVID-19
Эвакуационных мероприятий больных или лиц с подозрением на COVID-19 Патология аортального клапана
Патология аортального клапана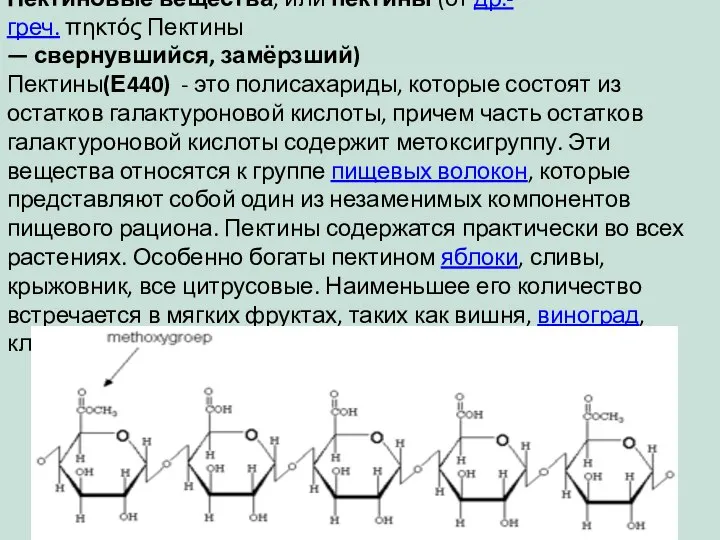 Пекти́новые вещества́,
Пекти́новые вещества́, Правовое регулирование трансплантологии
Правовое регулирование трансплантологии Патологии HEEL д-и. Депрессии экзогенные
Патологии HEEL д-и. Депрессии экзогенные Gnano: ощути вкус нанотехнологий. - презентация_
Gnano: ощути вкус нанотехнологий. - презентация_ Классификация медицинских отходов по степени их эпидемической, токсикологической и радиационной опасности
Классификация медицинских отходов по степени их эпидемической, токсикологической и радиационной опасности